Angiotensin-Converting Enzyme
From Proteopedia
| Line 61: | Line 61: | ||
During the SARS scare of 2002-2003, extensive research was focused on the interactions between the SARS virus and its host cells. It was determined that the severe acute respiratory syndrome conavirus (SARS-CoV) enters cells through the activities of a spike shaped protein on its outer envelope. <ref name="SARS">PMID:18448527</ref> The Receptor Binding Domain (RBD) of SARS-CoV binds to ACE2, on the surface of the cell. It was determined that by changing a few selected residues on either the SARS-CoV RBD or the ACE2 binding site, the virus becomes significantly more infectious. <scene name='Angiotensin-Converting_Enzyme/Sars/2'>It is believed that these mutations</scene> ([[3d0g]]), namely at residues 31, 35, 38, & 353 in ACE2 or residues 479 and 487 in the SARS-CoV RBD, are what allowed for SARS transmission from [http://en.wikipedia.org/wiki/Civet Civets] to Humans. In fact, in those SARS strains which were determined to be most infectious, the unfavorable electrostatic interactions at the binding interface were removed via mutations at the critical residues 479 and 487. <ref name="SARS"/> | During the SARS scare of 2002-2003, extensive research was focused on the interactions between the SARS virus and its host cells. It was determined that the severe acute respiratory syndrome conavirus (SARS-CoV) enters cells through the activities of a spike shaped protein on its outer envelope. <ref name="SARS">PMID:18448527</ref> The Receptor Binding Domain (RBD) of SARS-CoV binds to ACE2, on the surface of the cell. It was determined that by changing a few selected residues on either the SARS-CoV RBD or the ACE2 binding site, the virus becomes significantly more infectious. <scene name='Angiotensin-Converting_Enzyme/Sars/2'>It is believed that these mutations</scene> ([[3d0g]]), namely at residues 31, 35, 38, & 353 in ACE2 or residues 479 and 487 in the SARS-CoV RBD, are what allowed for SARS transmission from [http://en.wikipedia.org/wiki/Civet Civets] to Humans. In fact, in those SARS strains which were determined to be most infectious, the unfavorable electrostatic interactions at the binding interface were removed via mutations at the critical residues 479 and 487. <ref name="SARS"/> | ||
</StructureSection> | </StructureSection> | ||
| - | ==Additional 3D Structures of | + | ==Additional 3D Structures of Angiotensin-Converting Enzyme== |
[[1o8a]] – hANCE - human<br /> | [[1o8a]] – hANCE - human<br /> | ||
Revision as of 06:22, 9 May 2011
Template:STRUCTURE 1o8a
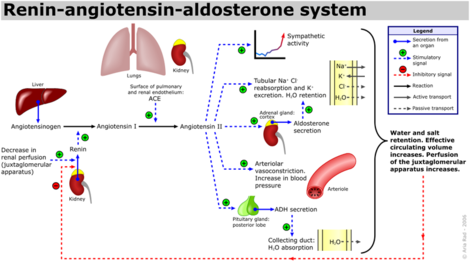
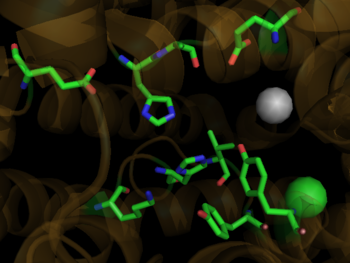
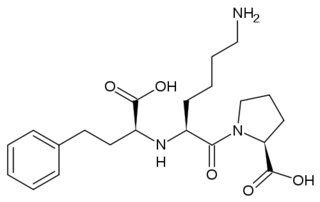
Angiotensin-Converting Enzyme (ACE) is both an exopeptidase and endopeptindase first discovered by Skeggs et al. in 1956. [1] ACE is a zinc- and chloride-dependent metallopeptidase that is responsible for the metabolism of key biologically active peptides, namely Angiotensin I and Bradykinin. These two peptides play a critical role in maintaining appropriate blood pressure in the human body along with a host of other homeostatic circulatory functions. ACE catalyzes the conversion of the decapeptide Angiostensin I to the octapeptide Angiostensin II. Due to its critical role in the Renin-Angiotensin-Aldosterone System (RAAS), ACE has been targeted by a number of pharmaceutical compounds to treat hypertension, diabetic nephropathy, and renal failure. [2]
Contents |
Biological Role
ACE is a Zn and Chloride dependent type-1 membrane protein (N-terminal regions are outside the cell). Two types of Angiotensin-converting enzyme exist, ACE1 and ACE2, although the most focus has been on ACE1 which has been attributed with receptor-mediated effects like vasoconstriction, inflammation and cell growth/proliferation. [3] The Renin-Angiotensin System (RAS) is a major regulator of blood pressure in the human body. Renin is an enzyme produced by the liver which cleaves Angiotensinogen into Angiotensin I Angiotensin Ihas the sequence, DRVTIHPFHL, and does not appear to have any biological activity. Angiotensin 1 (See:1n9u) is converted into Angiotensin II (See:1n9v) via the removal of the two C-terminal residues by ACE, yielding the active peptide: DRVTIHPF. [4]
Angiotensin II interacts with two receptor subtypes, AT1 and AT2, which are widely distributed throughout the body. [5] Binding of Angiotensin II to ATI leads to vasoconstriction by vascular smooth muscle cells, resulting in increased blood pressure, as well as the release of fluid and electrolyte homeostasis regulator, aldosterone, by the adrenal glands. Further, Angiotensin II binds to kidney AT1 receptors resulting in sodium ion reabsorption, leading to increased water retention in the blood and subsequent increased blood pressure. [6]
| Selected AT1 and AT2 Receptor-Mediated Effects of Angiotensin II. [7][3] | |
|---|---|
| AT1 Receptor Mediated Effects | AT2 Receptor Mediated Effects |
| Vasoconstriction | Vasodilation |
| Inflammation | Inflammation |
| Cell Growth and Proliferation | Apoptosis and Fibroblast Growth Inhibition |
| Cardiovascular effects: Increased Atherogenicity, increased arrhythmogenicity, decreased renal blood flow, increased myocardial contractility. | Cardiovascular Effects: Improved cardiac function and decreased chornotropic effect. |
Additionally, Bradykinin, which is inactivated by ACE1, has vasodilatory and cardioprotective properties by promoting the formation of nitric oxide by the endothelium. [8] The essential role ACE1 plays in blood pressure homeostasis is further supported by knockout mice created by Cole et. al. ACE1 knockout mice exhibited an approximate 35% reduction in blood pressure, resulting in hypotension and subsequent organ damage. Thus despite the many systems contributing to blood pressure in mammals, i.e. nitric oxide, endothelin and andregenic stimulation etc. these redundant systems are not enough to overcome a disruption of the RAAS. [9] It should be noted that AT2 binding of Angiotensin II results in many processes that counterbalance the binding of AT1. See the schematic image of the Renin-Angiotensin-Aldosterone System at the left for a visual description and the table below for selected Angiotensin receptor-mediated effects of binding Angiotensin II.
Structural Analysis, Mechanism, & Activation
| |||||||||||
Medical Implications
| |||||||||||
Additional 3D Structures of Angiotensin-Converting Enzyme
1o8a – hANCE - human
2iul, 2iux, 3nxq – hANCE (mutant)
2c6f – hANCE N domain
2c6n - hANCE N domain+lisinopril
1o86 - hANCE +lisinopril
3kbh, 3d0g, 3d0h, 3d0i, 2ajf – hANCE 2 fragment+spike glycoprotein
3l3n – hANCE+LISW
3bkk, 3bkl – hANCE+ketone inhibitor
2oc2 - hANCE+phosphinic inhibitor
1uze, 1uzf - hANCE+anti-hypertensive drug
2xhm – DmANCE+K26 – Drosophila melanogaster
2x8y – DmANCE
2x8z, 2x90, 2x91, 2x92, 2x95, 2x96, 2x97, 1j36, 1j37, 1j38 – DmANCE+anti-hypertensive drug
Additional Resources
For Additional Information, see: Hypertension & Congestive Heart Failure
References
- ↑ Skeggs, L. T., Dorer, F. E., Kahn, J. R., Lentz, K. E., Levin, M. (1981) Experimental renal hypertension: the discovery of the Renin-Angiotensin system. Soffer, R. eds. Biochemical Regulation of Blood Pressure ,3-38 John Wiley & Sons, Inc. Hoboken.
- ↑ Hoogwerf BJ, Young JB. The HOPE study. Ramipril lowered cardiovascular risk, but vitamin E did not. Cleve Clin J Med. 2000 Apr;67(4):287-93. PMID:10780101
- ↑ 3.0 3.1 3.2 Ferrario CM. Role of angiotensin II in cardiovascular disease therapeutic implications of more than a century of research. J Renin Angiotensin Aldosterone Syst. 2006 Mar;7(1):3-14. PMID:17083068
- ↑ Spyroulias GA, Nikolakopoulou P, Tzakos A, Gerothanassis IP, Magafa V, Manessi-Zoupa E, Cordopatis P. Comparison of the solution structures of angiotensin I & II. Implication for structure-function relationship. Eur J Biochem. 2003 May;270(10):2163-73. PMID:12752436
- ↑ 5.0 5.1 Brew K. Structure of human ACE gives new insights into inhibitor binding and design. Trends Pharmacol Sci. 2003 Aug;24(8):391-4. PMID:12915047
- ↑ 6.0 6.1 Sturrock ED, Natesh R, van Rooyen JM, Acharya KR. Structure of angiotensin I-converting enzyme. Cell Mol Life Sci. 2004 Nov;61(21):2677-86. PMID:15549168 doi:10.1007/s00018-004-4239-0
- ↑ 7.0 7.1 7.2 Weir MR. Effects of renin-angiotensin system inhibition on end-organ protection: can we do better? Clin Ther. 2007 Sep;29(9):1803-24. PMID:18035185 doi:10.1016/j.clinthera.2007.09.019
- ↑ Henriksen EJ, Jacob S. Modulation of metabolic control by angiotensin converting enzyme (ACE) inhibition. J Cell Physiol. 2003 Jul;196(1):171-9. PMID:12767053 doi:10.1002/jcp.10294
- ↑ Cole J, Ertoy D, Bernstein KE. Insights derived from ACE knockout mice. J Renin Angiotensin Aldosterone Syst. 2000 Jun;1(2):137-41. PMID:11967804
- ↑ Junot C, Gonzales MF, Ezan E, Cotton J, Vazeux G, Michaud A, Azizi M, Vassiliou S, Yiotakis A, Corvol P, Dive V. RXP 407, a selective inhibitor of the N-domain of angiotensin I-converting enzyme, blocks in vivo the degradation of hemoregulatory peptide acetyl-Ser-Asp-Lys-Pro with no effect on angiotensin I hydrolysis. J Pharmacol Exp Ther. 2001 May;297(2):606-11. PMID:11303049
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 Natesh R, Schwager SL, Sturrock ED, Acharya KR. Crystal structure of the human angiotensin-converting enzyme-lisinopril complex. Nature. 2003 Jan 30;421(6922):551-4. Epub 2003 Jan 19. PMID:12540854 doi:http://dx.doi.org/10.1038/nature01370
- ↑ Hangauer DG, Monzingo AF, Matthews BW. An interactive computer graphics study of thermolysin-catalyzed peptide cleavage and inhibition by N-carboxymethyl dipeptides. Biochemistry. 1984 Nov 20;23(24):5730-41. PMID:6525336
- ↑ Jaspard E, Alhenc-Gelas F. Catalytic properties of the two active sites of angiotensin I-converting enzyme on the cell surface. Biochem Biophys Res Commun. 1995 Jun 15;211(2):528-34. PMID:7794265
- ↑ http://www.yourlawyer.com/topics/overview/ace_inhibitors
- ↑ Natesh R, Schwager SL, Evans HR, Sturrock ED, Acharya KR. Structural details on the binding of antihypertensive drugs captopril and enalaprilat to human testicular angiotensin I-converting enzyme. Biochemistry. 2004 Jul 13;43(27):8718-24. PMID:15236580 doi:10.1021/bi049480n
- ↑ 16.0 16.1 Li F. Structural analysis of major species barriers between humans and palm civets for severe acute respiratory syndrome coronavirus infections. J Virol. 2008 Jul;82(14):6984-91. Epub 2008 Apr 30. PMID:18448527 doi:10.1128/JVI.00442-08
Proteopedia Page Contributors and Editors (what is this?)
David Canner, Michal Harel, Alexander Berchansky, Cristina Murga