Insulin
From Proteopedia
| Line 1: | Line 1: | ||
| - | Insulin is a | + | [[Image:Insulin.gif|right|Insulin chain A and B. For interactive figures, scroll down and click on green links]] |
| - | + | '''Insulin''' is a peptide hormone that helps to maintain blood sugar within a healthy range by regulating [[Carbohydrate Metabolism|carbohydrate]] and lipid metabolism throughout the body<ref>PMID:10927996</ref><ref>DOI:10.1111/dom.13402</ref>. It is secreted by specialized cells in the pancreas and acts by binding to [[insulin receptor|insulin receptors]] on other cells. Insulin in its mature form contains two peptide chains connected by disulfide crosslinks, and occurs either as monomer or as hexamer. Administering insulin in carefully determined doses at the appropriate times is used in managing [[diabetes]], a chronic condition where the body fails to maintain blood sugar levels by itself. | |
| + | ==Other Proteopedia pages about or relating to insulin== | ||
[[Diabetes & Hypoglycemia]]<br> | [[Diabetes & Hypoglycemia]]<br> | ||
| - | [[User:Karsten_Theis/Insulin]]<br> | ||
[[Insulin (Hebrew)]]<br> | [[Insulin (Hebrew)]]<br> | ||
[[Insulin glargine]]<br> | [[Insulin glargine]]<br> | ||
| Line 9: | Line 9: | ||
[[Insulin-Degrading Enzyme]]<br> | [[Insulin-Degrading Enzyme]]<br> | ||
[[Molecular_Playground/Insulin]]<br> | [[Molecular_Playground/Insulin]]<br> | ||
| - | [https://pdb101.rcsb.org/motm/14 Insulin @RCSB]<br> | ||
| - | [https://en.wikipedia.org/wiki/Insulin Insulin @Wikipedia]<br> | ||
| - | [http://www.ebi.ac.uk/pdbe/quips?story=insulin Insulin @PDBe]<br> | ||
| - | |||
| - | ==How does Insulin works?== | ||
[[Insulin Structure & Function]]<br> | [[Insulin Structure & Function]]<br> | ||
[[Insulin 3D Structures]]<br> | [[Insulin 3D Structures]]<br> | ||
| - | == | + | ====Proteins that interact with insulin==== |
[[Student Projects for UMass Chemistry 423 Spring 2012-1|Insulin Receptor UMAss]]<br> | [[Student Projects for UMass Chemistry 423 Spring 2012-1|Insulin Receptor UMAss]]<br> | ||
[[Insulin Receptor - kinase_domain (Hebrew)]]<br> | [[Insulin Receptor - kinase_domain (Hebrew)]]<br> | ||
| Line 23: | Line 18: | ||
[[Insulin-like growth factor receptor]]<br> | [[Insulin-like growth factor receptor]]<br> | ||
| - | ==Tutorials== | + | ====Tutorials we would love to see==== |
Tutorial: what molecules play a role in diabetes? (TBD) <span class="fas fa-user-md" style="color:#32CD32"></span> <span class="fas fa-user-graduate" style="color:#32CD32"></span><br> | Tutorial: what molecules play a role in diabetes? (TBD) <span class="fas fa-user-md" style="color:#32CD32"></span> <span class="fas fa-user-graduate" style="color:#32CD32"></span><br> | ||
Tutorial: how does insulin regulate my blood sugar? (TBD) <span class="fas fa-child" style="color:#32CD32"></span><span class="fas fa-chalkboard-teacher" style="color:#32CD32"></span><br> | Tutorial: how does insulin regulate my blood sugar? (TBD) <span class="fas fa-child" style="color:#32CD32"></span><span class="fas fa-chalkboard-teacher" style="color:#32CD32"></span><br> | ||
| + | |||
| + | ==Function== | ||
| + | |||
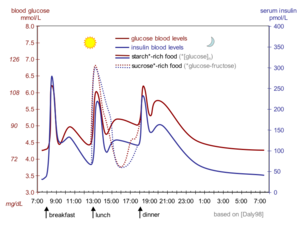
| + | [[Image:Glucose insulin day.png|300px|left|thumb|Schematic of daily changes of blood sugar (red) and insulin (blue)]] | ||
| + | Our blood sugar level (i.e. glucose concentration) varies over time with food intake and exercise, but has to remain in a narrow range so we stay healthy (not become hyperglycemic or hypoglycemic). Insulin, together with [[glucagon]], regulates blood sugar levels by changing fuel metabolism in all cells <ref>https://www.yourhormones.info/hormones/insulin/</ref> on a timescale of minutes and hours. In simplest terms, the presence of insulin in the blood signals the well-fed stage, while the presence of glucagon signals the fasting stage. | ||
| + | |||
| + | Biosynthesis and processing of insulin occurs in the [https://en.wikipedia.org/wiki/Beta_cell beta cells] of the pancreas. The beta cells are found in the islets of Langerhans, which also contain the alpha cells that synthesize glucagon. Insulin is made as a 110 amino acid pre-proinsulin, which is processed to the mature 51 amino acid insulin and targeted to secretory vesicles. In a healthy adult, about 200 units of insulin are available in the pancreas, of which 30-50 units are secreted daily<ref>https://www.britannica.com/science/insulin</ref>. With a unit of insulin corresponding to 0.0347 mg mature insulin <ref>https://www.who.int/biologicals/expert_committee/BS_2143_Human_Recombinant_Insulin_final.pdf</ref>, the body contains only about 7 mg of insulin. In its stored form, insulin is a hexamer complexed to zinc ions. | ||
| + | |||
| + | Insulin is constantly released into the blood stream at a basal level. When blood glucose levels rise after a meal containing carbohydrates (sugars and starches), increased intracellular glucose in the beta cells triggers a series of processes that change the intracellular calcium concentration. First, the calcium concentration rises and stays elevated for 5-10 minutes, and then it spikes in intervals of roughly 3 minutes. Whenever calcium concentrations are high, insulin-containing vesicles merge with the plasma membrane, releasing insulin into the blood stream in the same temporal pattern as the calcium spikes<ref>DOI: 10.1007/s00125-009-1314-y</ref>. The insulin is released into the bloodstream, where it first reaches the liver via the portal vein<ref>"https://www.diabetesselfmanagement.com/diabetes-resources/definitions/portal-vein/"</ref>, and then the other organs after insulin-containing blood returns from the heart. | ||
| + | |||
| + | [[Image:Insulin receptor cartoon.gif|frame|Artist's conception of insulin receptor (purple) binding to insulin outside of the cell and being phosphorylated inside of the cell]]Liver cells and other cells contain [[insulin receptor|receptors]] with insulin binding sites on the cell surface. These intermembrane receptors<ref>https://pdb101.rcsb.org/motm/182</ref> change conformation upon insulin binding, activating intracellular tyrosine kinase domains<ref name="gutmann">DOI: 10.1083/jcb.201711047</ref>. This starts a signalling cascade within the cell that changes glucose uptake as well as carbohydrate and lipid metabolism. The liver stores available glucose in the form of glycogen and, when there is additional glucose, converts it into fatty acids and carbon dioxide. Cells in other organs (e.g. adipose tissue, muscles) also alter their metabolism depending on insulin levels. | ||
| + | |||
| + | Once insulin binds to its receptor, the receptor is removed from the plasma membrane, insulin is degraded and the receptor is recycled<ref>PMID:28974775</ref>. The majority of insulin is removed from the bloodstream this way on its first pass through the liver. The half-life of insulin in the blood plasma is about about 4-6 minutes<ref>DOI:10.1210/edrv.19.5.0349</ref>. | ||
| + | |||
| + | ==Disease and Treatment== | ||
| + | In patients with diabetes, insulin signalling is compromised<ref>https://www.endotext.org/section/diabetes/</ref>. In type I diabetes, insulin is not produced sufficiently because the beta cells in the pancreas are absent or compromised by an autoimmune event. The onset of type 1 diabetes is rapid, and often occurs early in life ("juvenile diabetes"). In type II diabetes, insulin is secreted at normal or even elevated levels, but the target cells do not respond properly, for reasons not yet understood<ref>DOI:10.1172/JCI77812</ref>. The onset of type 2 diabetes is gradual (over years), and there are warning signs (like insulin resistance) that in some cases helps to avert the onset by certain changes in lifestyle and diet<ref> DOI:10.1530/endoabs.56.PL5</ref>. | ||
| + | |||
| + | Type 1 diabetes is managed by administering insulin. The challenge is to keep the blood sugar level in a healthy range while conditions change (food intake, exercise, illness). Insulin can not be given orally because it is broken down in the digestive tract. Instead, it is administered via subcutaneous depots or in other non-oral forms). There are long-acting and short-acting preparations of insulin to provide the basal level and to manage spikes in blood glucose levels, respectively. Type 2 diabetes is managed in a variety of ways, which may include administration of extra insulin to partially counteract the diminished signalling capacity. | ||
| + | |||
| + | == Structure == | ||
| + | <StructureSection load='' size='350' side='right' scene='82/821037/Ribbon/1' caption=''> | ||
| + | ===Structure of mature insulin monomer=== | ||
| + | <scene name='82/821037/Ribbon/1'>Mature insulin</scene> contains two chains, A and B, held together by disulfide bonds and non-covalent interactions. The <scene name='82/821037/Spacefilling/2'>surface of insulin</scene> contains quite a few hydrophobic side chains, which form protein:protein contacts when insulin forms hexamers or binds to its receptor. Select coloring of the side chains below to explore the surface properties. | ||
| + | |||
| + | Sidechains colored by <jmol> | ||
| + | <jmolRadioGroup> | ||
| + | <item> | ||
| + | <script>background white; select sidechain; color magenta; select sidechain and (cys, met, ile, leu, val, phe, tyr, trp); color gray; set echo OFF; set echo ID bla 80% 0%; echo "hydrophobic"; color echo gray; frank off; set echo ID bla2 0% 0%; echo "hydrophilic"; color echo magenta </script> | ||
| + | <text>hydrophobiticity</text> | ||
| + | <checked>false</checked> | ||
| + | </item> | ||
| + | <item> | ||
| + | <script>select sidechain; color white; select sidechain and (asp, glu); color red; select sidechain and (lys, arg, his); color blue; set echo OFF; set echo ID bla 80% 0%; echo "positive"; color echo blue; frank off; set echo ID bla2 0% 0%; echo "negative"; color echo red</script> | ||
| + | <text>charge</text> | ||
| + | <checked>false</checked> | ||
| + | </item> | ||
| + | <item> | ||
| + | <script> select sidechain; color cpk;set echo OFF; set echo ID bla 80% 0%; echo "oxygen"; color echo red; frank off; set echo ID bla2 0% 0%; echo "nitrogen"; color echo blue; set echo ID bla4 25% 0%; echo "sulfur"; color echo gold; set echo ID bla3 55% 0%; echo "carbon"; color echo gray;</script> | ||
| + | <text>element</text> | ||
| + | <checked>true</checked> | ||
| + | </item> | ||
| + | </jmolRadioGroup> | ||
| + | </jmol> | ||
| + | |||
| + | ===Targeting and processing=== | ||
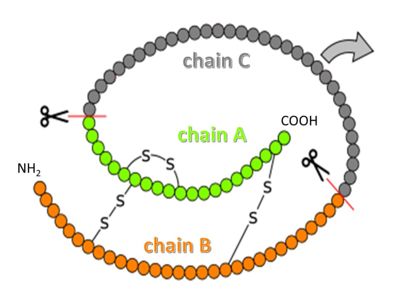
| + | [[Image:Proinsulin.jpg|400 px]] | ||
| + | |||
| + | Insulin it synthesized as so-called preproinsulin and gets targeted into the ER and Golgi via a signal sequence, which then is removed to yield proinsulin. <scene name='82/821037/Proinsulin/1'>Proinsulin</scene> is processed by several proteases in the Golgi apparatus to form 3 separate chains, named B, C and A (see figure above)<ref>PMID:15289650</ref>. Chains B and A are linked through disulfide bonds, and are the components of mature insulin. | ||
| + | |||
| + | <jmol> | ||
| + | <jmolRadioGroup> | ||
| + | <item> | ||
| + | <script> select (29-64); backbone off; </script> | ||
| + | <text>mature insulin</text> | ||
| + | <checked>false</checked> | ||
| + | </item> | ||
| + | <item> | ||
| + | <script> select (29-64); backbone on; </script> | ||
| + | <text>proinsulin</text> | ||
| + | <checked>false</checked> | ||
| + | </item> | ||
| + | </jmolRadioGroup> | ||
| + | </jmol> | ||
| + | |||
| + | |||
| + | Chain C, flexible and somewhat <jmol> | ||
| + | <jmolLink> | ||
| + | <script>anim mode loop; anim on</script> | ||
| + | <text>disordered</text></jmolLink></jmol> in the proinsulin structure, is no longer connected to insulin after processing and its fate and biological role after processing is unclear. | ||
| + | |||
| + | ===Storage=== | ||
| + | Before insulin is secreted, it is able to pair-up with itself and form a dimer by forming hydrogen bonds between the ends of two B-chains, which then combine in threes to form a hexamer (a trimer of dimers to be exact). In crystal structures, insulin occurs in two states, <scene name='82/821037/Rvst/1'>T or R</scene>. In an <scene name='82/821037/Rvst/2'>animation</scene> (takes long to load), you can see the conformational change in chain B while maintaining the organisation of the dimer. | ||
| + | |||
| + | (A) <scene name='82/821037/T6/1'>T6 hexamer (e.g. structure 4INS) </scene>, (B) T3Rf3 hexamer (e.g. 1TRZ) and (C) R6 hexamer (e.g. 1ZNJ). Small changes in the sequence of insulin change how fast hexamers fall apart into monomers. This is used to make insulin preparations that give off low levels of insulin for a longer time, or high levels of insulin for a short time when injected as microcrystals in depots under the skin. | ||
| + | |||
| + | ===Receptor interaction=== | ||
| + | The insulin receptor belongs to the class of tyrosine kinase receptors. Many of these receptors occur as monomers that dimerize upon ligand binding, bringing the intracellular tytrosine kinase domains (the endodomains) into close vicinity. In contrast, the insulin receptor (just like the closely related IGF-1 receptor) is a dimer even in the absence of ligand, crosslinked by disulfide bridges. The unliganded receptor ectodomain has the shape of a Λ (an inverted V), keeping the transmembrane segments and the endodomains at a distance. | ||
| + | |||
| + | Cryo-electronmicroscopy studies have shown a [http://proteopedia.org/wiki/images/0/05/LambdaTee.gif Λ to T transition] when insulin binds. One structure resolves four <scene name='82/821037/Spacefilling/5'>insulin binding sites</scene> (1, 1', 2, 2') per receptor dimer<ref name="ecto">DOI:10.1101/679233 </ref> (coordinates not yet available). Contacts with insulin are distinct in site 1 vs. site 2, as are the conformations of insulin. For comparison to the initial scene, here is another view of the <scene name='82/821037/Ribbon/2'>contact residues</scene>. | ||
| + | |||
| + | <scene name='82/821037/Receptor_bound/1'>Binding sites 1 and 1'</scene> had already been characterized in previous structures<ref>PMID:29512653</ref><ref name="gutmann"/>. Insulin makes contacts with both the N-terminal domain and the CT alpha helix, structural elements that are far apart in the unliganded conformation. Thus, binding of insulin in site 1 requires a large structural rearrangement that activates the tyrosine kinase activity of the endodomain by bringing the two kinase domains close for autophosphorylation. | ||
| + | |||
| + | </StructureSection> | ||
| + | |||
| + | ==See also== | ||
| + | [https://pdb101.rcsb.org/motm/14 Insulin @RCSB]<br> | ||
| + | [https://en.wikipedia.org/wiki/Insulin Insulin @Wikipedia]<br> | ||
| + | [http://www.ebi.ac.uk/pdbe/quips?story=insulin Insulin @PDBe]<br> | ||
| + | [http://pdb101.rcsb.org/browse/diabetes Diabetes @RCSB] | ||
| + | |||
| + | == References == | ||
| + | <references/> | ||
Revision as of 19:50, 16 July 2019
Insulin is a peptide hormone that helps to maintain blood sugar within a healthy range by regulating carbohydrate and lipid metabolism throughout the body[1][2]. It is secreted by specialized cells in the pancreas and acts by binding to insulin receptors on other cells. Insulin in its mature form contains two peptide chains connected by disulfide crosslinks, and occurs either as monomer or as hexamer. Administering insulin in carefully determined doses at the appropriate times is used in managing diabetes, a chronic condition where the body fails to maintain blood sugar levels by itself.
Contents |
Other Proteopedia pages about or relating to insulin
Diabetes & Hypoglycemia
Insulin (Hebrew)
Insulin glargine
Insulin and pro-insulin (Hebrew)
Insulin-Degrading Enzyme
Molecular_Playground/Insulin
Insulin Structure & Function
Insulin 3D Structures
Proteins that interact with insulin
Insulin Receptor UMAss
Insulin Receptor - kinase_domain (Hebrew)
Insulin receptor
Insulin-like growth factor receptor
Tutorials we would love to see
Tutorial: what molecules play a role in diabetes? (TBD)
Tutorial: how does insulin regulate my blood sugar? (TBD)
Function
Our blood sugar level (i.e. glucose concentration) varies over time with food intake and exercise, but has to remain in a narrow range so we stay healthy (not become hyperglycemic or hypoglycemic). Insulin, together with glucagon, regulates blood sugar levels by changing fuel metabolism in all cells [3] on a timescale of minutes and hours. In simplest terms, the presence of insulin in the blood signals the well-fed stage, while the presence of glucagon signals the fasting stage.
Biosynthesis and processing of insulin occurs in the beta cells of the pancreas. The beta cells are found in the islets of Langerhans, which also contain the alpha cells that synthesize glucagon. Insulin is made as a 110 amino acid pre-proinsulin, which is processed to the mature 51 amino acid insulin and targeted to secretory vesicles. In a healthy adult, about 200 units of insulin are available in the pancreas, of which 30-50 units are secreted daily[4]. With a unit of insulin corresponding to 0.0347 mg mature insulin [5], the body contains only about 7 mg of insulin. In its stored form, insulin is a hexamer complexed to zinc ions.
Insulin is constantly released into the blood stream at a basal level. When blood glucose levels rise after a meal containing carbohydrates (sugars and starches), increased intracellular glucose in the beta cells triggers a series of processes that change the intracellular calcium concentration. First, the calcium concentration rises and stays elevated for 5-10 minutes, and then it spikes in intervals of roughly 3 minutes. Whenever calcium concentrations are high, insulin-containing vesicles merge with the plasma membrane, releasing insulin into the blood stream in the same temporal pattern as the calcium spikes[6]. The insulin is released into the bloodstream, where it first reaches the liver via the portal vein[7], and then the other organs after insulin-containing blood returns from the heart.
Once insulin binds to its receptor, the receptor is removed from the plasma membrane, insulin is degraded and the receptor is recycled[10]. The majority of insulin is removed from the bloodstream this way on its first pass through the liver. The half-life of insulin in the blood plasma is about about 4-6 minutes[11].
Disease and Treatment
In patients with diabetes, insulin signalling is compromised[12]. In type I diabetes, insulin is not produced sufficiently because the beta cells in the pancreas are absent or compromised by an autoimmune event. The onset of type 1 diabetes is rapid, and often occurs early in life ("juvenile diabetes"). In type II diabetes, insulin is secreted at normal or even elevated levels, but the target cells do not respond properly, for reasons not yet understood[13]. The onset of type 2 diabetes is gradual (over years), and there are warning signs (like insulin resistance) that in some cases helps to avert the onset by certain changes in lifestyle and diet[14].
Type 1 diabetes is managed by administering insulin. The challenge is to keep the blood sugar level in a healthy range while conditions change (food intake, exercise, illness). Insulin can not be given orally because it is broken down in the digestive tract. Instead, it is administered via subcutaneous depots or in other non-oral forms). There are long-acting and short-acting preparations of insulin to provide the basal level and to manage spikes in blood glucose levels, respectively. Type 2 diabetes is managed in a variety of ways, which may include administration of extra insulin to partially counteract the diminished signalling capacity.
Structure
| |||||||||||
See also
Insulin @RCSB
Insulin @Wikipedia
Insulin @PDBe
Diabetes @RCSB
References
- ↑ Sonksen P, Sonksen J. Insulin: understanding its action in health and disease. Br J Anaesth. 2000 Jul;85(1):69-79. PMID:10927996
- ↑ Weiss MA, Lawrence MC. A thing of beauty: Structure and function of insulin's "aromatic triplet". Diabetes Obes Metab. 2018 Sep;20 Suppl 2:51-63. doi: 10.1111/dom.13402. PMID:30230175 doi:http://dx.doi.org/10.1111/dom.13402
- ↑ https://www.yourhormones.info/hormones/insulin/
- ↑ https://www.britannica.com/science/insulin
- ↑ https://www.who.int/biologicals/expert_committee/BS_2143_Human_Recombinant_Insulin_final.pdf
- ↑ Henquin JC. Regulation of insulin secretion: a matter of phase control and amplitude modulation. Diabetologia. 2009 May;52(5):739-51. doi: 10.1007/s00125-009-1314-y. Epub 2009, Mar 14. PMID:19288076 doi:http://dx.doi.org/10.1007/s00125-009-1314-y
- ↑ "https://www.diabetesselfmanagement.com/diabetes-resources/definitions/portal-vein/"
- ↑ https://pdb101.rcsb.org/motm/182
- ↑ 9.0 9.1 Gutmann T, Kim KH, Grzybek M, Walz T, Coskun U. Visualization of ligand-induced transmembrane signaling in the full-length human insulin receptor. J Cell Biol. 2018 May 7;217(5):1643-1649. doi: 10.1083/jcb.201711047. Epub 2018, Feb 16. PMID:29453311 doi:http://dx.doi.org/10.1083/jcb.201711047
- ↑ Haeusler RA, McGraw TE, Accili D. Biochemical and cellular properties of insulin receptor signalling. Nat Rev Mol Cell Biol. 2018 Jan;19(1):31-44. doi: 10.1038/nrm.2017.89. Epub 2017 , Oct 4. PMID:28974775 doi:http://dx.doi.org/10.1038/nrm.2017.89
- ↑ Duckworth WC, Bennett RG, Hamel FG. Insulin degradation: progress and potential. Endocr Rev. 1998 Oct;19(5):608-24. doi: 10.1210/edrv.19.5.0349. PMID:9793760 doi:http://dx.doi.org/10.1210/edrv.19.5.0349
- ↑ https://www.endotext.org/section/diabetes/
- ↑ Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. J Clin Invest. 2016 Jan;126(1):12-22. doi: 10.1172/JCI77812. Epub 2016 Jan 4. PMID:26727229 doi:http://dx.doi.org/10.1172/JCI77812
- ↑ doi: https://dx.doi.org/10.1530/endoabs.56.PL5
- ↑ Davidson HW. (Pro)Insulin processing: a historical perspective. Cell Biochem Biophys. 2004;40(3 Suppl):143-58. PMID:15289650
- ↑ doi: https://dx.doi.org/10.1101/679233
- ↑ Scapin G, Dandey VP, Zhang Z, Prosise W, Hruza A, Kelly T, Mayhood T, Strickland C, Potter CS, Carragher B. Structure of the Insulin Receptor-Insulin Complex by Single Particle CryoEM analysis. Nature. 2018 Feb 28. pii: nature26153. doi: 10.1038/nature26153. PMID:29512653 doi:http://dx.doi.org/10.1038/nature26153
Proteopedia Page Contributors and Editors (what is this?)
Karsten Theis, Michal Harel, Alexander Berchansky, Jaime Prilusky, David Canner