User:Marvin O'Neal/OspA
From Proteopedia
m (Studio:G2SecL03 moved to User:Marvin O'Neal/OspA) |
|||
| (88 intermediate revisions not shown.) | |||
| Line 1: | Line 1: | ||
| - | + | <Structure load="1fj1" size="350" frame="true" align="right" name="OspA-secondary" caption="Outer surface protein A (OspA) ([[1fj1|1FJ1]], chain F) showing secondary structures." scene="Studio:G2SecL03/Ospa_default/5"/> | |
| + | <p> | ||
| + | <b>Outer Surface Protein A (OspA)</b> is a major lipoprotein found on the surface of [http://en.wikipedia.org/wiki/Spirochaete spirochetes] from the genus [http://en.wikipedia.org/wiki/Borrelia <i>Borrelia</i>] and is comprised of 21 anti-parallel β-sheets and a single α-helix. OspA's expression is regulated at different points in time, from being downregulated during the tick's feeding process on its host to being upregulated in the host's cerebrospinal fluid (CSF) to induce inflammatory response, resulting in acute Lyme [http://en.wikipedia.org/wiki/Neuroborreliosis neuroborreliosis]. OspA has also been used as a vector in working towards the development of a vaccine for [http://en.wikipedia.org/wiki/Lyme_disease Lyme disease]. | ||
| + | </p> | ||
| - | <b>Hello world</b> <u>This is a test.</u> <i>Protein Model test</i> | ||
| - | this is andrea testing | ||
| - | <Structure load="1fj1" size="400" frame="true" align="right" caption="Insert caption here" scene="Studio:G2SecL03/Ospa_default/4"/> | ||
| - | + | <h2>Introduction</h2> | |
| - | + | ||
<p> | <p> | ||
| - | < | + | Lyme disease is caused by the spirochete <i>Borrelia</i> and spread via hard-bodied ticks belonging to the family [http://en.wikipedia.org/wiki/Ixodidae <i>Ixodidae</i>]. The <i>Borrelia</i> spirochetes are motile, helical organisms have several lipoproteins exposed on the surfaces of their membranes that invoke a response from host immune systems. The predominant group of these is classified as the outer surface proteins (Osps). Both the pathogenesis of Lyme disease as well as the host's immune response stem from the effects of the spirochete's presence and involvement in the system.<ref name="connolly">PMID: 15864264</ref> |
| - | Lyme disease | + | |
| - | < | + | The major strain of <i>Borrelia</i> in the United States is [http://en.wikipedia.org/wiki/Borrelia_burgdorferi <i>Borrelia burgdorferi</i>] <i>sensu stricto (Bb.)</i>, with 20-100 cases of Lyme disease being reported per 100,000 people. In Europe, Lyme disease cases are more prevalent, with 100-130 diagnoses per 100,000 people, but are caused by the spirochetes [http://en.wikipedia.org/wiki/Borrelia_afzelii <i>Borrelia afzelii (Ba.)</i>] and [http://en.wikipedia.org/wiki/Borrelia_garinii <i>Borrelia garinii (Bg.)</i>] in addition to <i>B. burgdorferi</i>.<ref name="rupprecht">PMID: 18097481</ref><ref name="ding">PMID: 11183781</ref> |
| - | OspA | + | </p> |
| - | There are three loops | + | <p> |
| + | Lyme disease is a debilitating condition that begins with a characteristic bullseye rash known as an [http://en.wikipedia.org/wiki/Erythema_chronicum_migrans erythema migrans (EM)] as well as the development of lesions on other parts of the body, not just at the site of the tick's attachment to its host. Secondary stage symptoms include affecting the heart, joints, and both the central and peripheral nervous systems. OspA is used in adhering to the tick's gut by binding with the tick receptor for OspA (TROSPA), a receptor necessary for the colonization of <i>Borrelia</i> inside the tick. High levels of both OspA and TROSPA are found prior to feeding, but are downregulated once the feeding process begins in order to initiate transmission into the host.<ref name="pal">PMID: 15537536</ref> | ||
| + | </p> | ||
| + | <p> | ||
| + | While feeding, OspA is downregulated in order to evade an immune response from the incoming host blood into the gut, releasing the <i>Borrelia</i> from the gut wall and migrating into the tick's salivary glands, thereby allowing it to enter the host through the bite. This is evidenced by the fact that patients with Lyme disease have been found to not possess OspA antibodies in the early stages of the disease.<ref name="connolly">PMID: 15864264</ref><ref name="rupprecht">PMID: 18097481</ref> OspA is the protein most related to acute Lyme neuroborreliosis (LNB), the neurological manifestations of Lyme disease. | ||
| + | </p> | ||
| + | |||
| + | |||
| + | |||
| + | <h2>OspA's Role in Invasion</h2> | ||
| + | <p> | ||
| + | Once inside the host, the <i>Borrelia</i> has a great number of mechanisms available to actively suppress the host's immune system response and neutralize its effector mechanisms, such as the expression of another outer surface protein, OspC, which prevents susceptibility to the host's [http://en.wikipedia.org/wiki/Innate_immune_system innate immunity] and [http://en.wikipedia.org/wiki/Complement_system complement systems]. Additionally, <i>Borrelia</i> is capable of suppressing many of its surface proteins to reduce its detectability, but can also utilize protective means by temporarily expressing them when needed. | ||
| + | </p> | ||
| + | |||
| + | <h3>Acute Lyme Neuroborreliosis (LNB)</h3> | ||
| + | <p> | ||
| + | Acute Lyme Neuroborreliosis (LNB) is part of the second stage of Lyme disease in which the spirochete invades the peripheral and central nervous systems (CNS). Symptoms of LNB include: meningoradiculitis with inflammation of the nerve roots and [http://en.wikipedia.org/wiki/Radicular_pain radiculitis] (Bannwarth’s syndrome), lymphocytic meningitis, and cranial and [http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001619/ peripheral neuritis]. In Europe, the strain predominantly found in the CSF of patients with Bannwarth's syndrome is <i>B. garinii</i>. However, in the United States, Bannwarth's syndrome is rare and the most common manifestations of Lyme neuroborreliosis is [http://en.wikipedia.org/wiki/Meningitis meningitis], caused by <i>B. burgdorferi</i>. The presence of OspA in the cerebrospinal fluid (CSF) is responsible for this complex inflammatory response in the brain that leads to the neuroborreliosis.<ref name="rupprecht">PMID: 18097481</ref> | ||
| + | </p> | ||
| + | |||
| + | <h3>Evasion and the Extracellular Matrix</h3> | ||
| + | <p> | ||
| + | The <i>Borrelia</i> are able to hide in the [http://en.wikipedia.org/wiki/Extracellular_matrix extracellular matrix], allowing it to survive by avoiding [http://en.wikipedia.org/wiki/Leukocytes leukocytes] circulating in the bloodstream. OspA can rapidly bind to plasminogen, which becomes [http://en.wikipedia.org/wiki/Plasmin plasmin] once activated, and degrades the extracellular matrix. By binding to plasminogen, <i>Borrelia</i> could be exploiting its function and utilizing it to invade the extracellular matrix. However, due to the fact that OspA is downregulated during feeding, and stays unexpressed, a different mechanism may be used instead. Additionally, <i>Borrelia</i> induces the local upregulation of matrix metalloproteinase-9, causing the digestion of the surrounding extracellular matrix. <i>Borrelia</i> can also bind to several proteins in the extracellular matrix, such as [http://en.wikipedia.org/wiki/Fibronectin fibronectin], [http://en.wikipedia.org/wiki/Integrins integrins] or [http://en.wikipedia.org/wiki/Decorin decorin], which can aid in the spread and survival of the spirochetes in these tissues.<ref name="rupprecht">PMID: 18097481</ref> | ||
| + | </p> | ||
| + | |||
| + | <h3>Migration Across the Blood-Brain Barrier</h3> | ||
| + | <p> | ||
| + | It is not fully understood how <i>Borrelia</i> get past the [http://en.wikipedia.org/wiki/Blood-brain_barrier blood-brain barrier], though some researchers suggest a paracellular route, which involves a process using transient tether-type associations, short-term dragging interactions, and stationary adhesion. There is evidence that <i>Borrelia</i> utilizes OspA in the transient tethering stage. The blood-brain barrier is composed of brain microvascular endothelial cells, astrocytes, a basement membrane, pericytes, and neurons. OspA is a major adherent molecule to brain microvascular cells by binding to the [[1aly|CD40]] receptors outside, which results in events that are typically seen when leukocytes cross the blood brain barrier. | ||
| + | |||
| + | Activation of CD40 receptors leads to the production of proinflammatory cytokines and enhanced expression of ICAM-1, E-selectin and VCAM-1, resulting in increased cell binding, and the formation of fenestrations due to increased vascular endothelial growth factor, and vascular permeability factor. OspA might be mimicking leukocytes in order to cross the blood-brain barrier. However not all strains of <i>Borrelia</i> can utilize OspA to do this, OspA only contributes about 70% to adherence, and other <i>Borrelia</i> proteins are also needed in this process. It has also been seen that OspA mediates the adhesion of <i>Borrelia</i> to murine neural and glial cell lines. <ref name="pulzova">PMID: 22355605</ref> | ||
| + | </p> | ||
| + | |||
| + | <h3>Role in Inflammation</h3> | ||
| + | |||
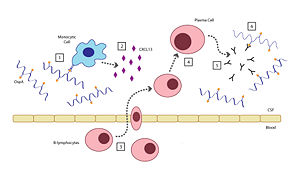
| + | [[Image:G2L03-OspA-mechanism.jpg|thumb|300px|Mechanism of the host inflammatory response to OspA]] | ||
| + | |||
| + | There are six steps involved in the host's inflammatory response to OspA: <ref name="rupprecht">PMID: 18097481</ref><br> | ||
| + | <ol> | ||
| + | <li>When the <i>Borrelia</i> enter the host’s CNS they encounter several different types of immune cells such as [http://en.wikipedia.org/wiki/Monocyte monocytes], [http://en.wikipedia.org/wiki/Macrophages macrophages], and [http://en.wikipedia.org/wiki/Dendritic_cells dendritic cells]. While in the CSF, outer surface protein A (OspA) is upregulated and it’s increased expression promotes recognition by a specific receptor on a monocyte.</li> | ||
| + | |||
| + | <li>The OspA-bound monocyte then releases proinflammatory [http://en.wikipedia.org/wiki/Cytokine cytokines] (i.e. [http://en.wikipedia.org/wiki/Interferon interferon]), as well as [http://en.wikipedia.org/wiki/Chemokine chemokines], such as [http://en.wikipedia.org/wiki/CXCL13 CXCL13]. In patients with LNB, there is an observed increase in the levels of these cytokines and chemokines in their CSF. The production of chemokines leads to the recruitment of other immune cells to the site of infection.</li> | ||
| + | |||
| + | <li>[http://en.wikipedia.org/wiki/B_lymphocyte B-lymphocytes] respond to the new concentration gradient of CXCL13 between the blood and CSF and migrate into the CSF.</li> | ||
| + | |||
| + | <li>B-lymphocytes undergo [http://en.wikipedia.org/wiki/Receptor-mediated_endocytosis receptor-mediated endocytosis], consuming the OspA antigens present in the CSF, thereby triggering its activation. The B-lymphocytes then are able to differentiate and mature into [http://en.wikipedia.org/wiki/Plasma_cells plasma cells].</li> | ||
| + | |||
| + | <li>The plasma cells create large quantities of anti-OspA antibodies specific to this strain of <i>Borrelia</i> and release them into the CSF.</li> | ||
| + | |||
| + | <li>The anti-OspA antibodies will then bind to the OspA on the spirochete’s membrane, thus killing the <i>Borrelia</i>.</li> | ||
| + | </ol> | ||
| + | |||
| + | <p> | ||
| + | This process is two-sided in the sense that the OspA aids in the pathogenesis of new symptoms (neuroborreliosis) through the chemokine’s actions, as well as initiating the signaling cascade to destroy itself. | ||
| + | </p> | ||
| + | |||
| + | |||
| + | |||
| + | <h2>OspA Vaccination</h2> | ||
| + | |||
| + | <Structure load="1fj1" size="350" frame="true" align="right" name="complex" caption="Outer surface protein A (OspA) in complex with the LA-2 Fab antibody ([[1fj1|1FJ1]])." scene="Studio:G2SecL03/Ospafab-orig/3"/> | ||
| + | |||
| + | <p> | ||
| + | Risk of developing Lyme disease can be mitigated by staying clear of areas with populations of ticks, wearing proper attire to minimize easily bitten areas of the body, and using insect repellents containing [http://en.wikipedia.org/wiki/DEET DEET] (N,N-diethy-m-toluamide). However, another effective means for prevention could be possible by using an outer surface protein from <i>Borrelia</i> in the creation of a vaccine.<ref name="nigrovic">PMID: 16893489</ref> | ||
| + | </p> | ||
| + | <p> | ||
| + | The membrane composition of <i>Borrelia</i> is abundant in both OspA and OspB, and the two proteins share a 53% similarity in their primary sequences. Both OspA and OspB are expressed in the tick's gut and downregulated during feeding and aid in its survivability; however, OspA is overall less varied and reactive than OspB, which has greater variability.<ref name="becker">PMID: 15713683</ref> The relatively conserved sequence of OspA thus lends itself better to study and application toward the development of a vaccine for a broader range of <i>Borrelia</i> strains in the treatment of Lyme disease than that of OspB. The first vaccine used a purified recombinant form of OspA and functioned in blocking transmission of the spirochetes expressing OspA from tick to host during feeding, killing them while still attached to the tick's gut.<ref name="connolly">PMID: 15864264</ref><ref name="battisti">PMID: 18779341</ref> The vaccine, Lymerix, had shown 76% and 92% effectiveness in separate clinical trials in which patients were treated for two years following a three-dose schedule. However, the vaccination was suspended from use in 2002 when opponents claimed the [http://en.wikipedia.org/wiki/Immunoglobulin_G IgG antibodies] for OspA were associated with the onset of severe chronic arthritis, as well as other side effects affecting immunity.<ref name="connolly">PMID: 15864264</ref><ref name="plotkin">PMID: 21217175</ref> This fact, in conjunction with the desire for a more widespread vaccine treating multiple strains of <i>Borrelia</i>, has spurred research towards a new vaccine. | ||
| + | </p> | ||
| + | <p> | ||
| + | To address the concerns of vaccine with broader protection, creation of a chimera, mixing the OspA of different strains of <i>Borrelia</i> would be ideal. Study of the epitope of <scene name='Studio:G2SecL03/Ospafab-ospa/3' target="complex">OspA</scene> and its <scene name='Studio:G2SecL03/Ospafab-interaction/3' target="complex">interactions</scene> with the murine monoclonal antibody <scene name='Studio:G2SecL03/Ospafab-fab/3' target="complex">LA-2</scene> have proved useful in determining effectiveness of a given vaccine trial as high levels of antibodies in test sera compete against LA-2 for binding with OspA. LA-2 makes direct contact with three exposed loops of the C-terminus of OspA. The recognition of OspA by LA-2 requires an induced fit mechanism where these three loops undergo conformational changes to optimize their interaction in the complex. <ref name="ding">PMID: 11183781</ref> | ||
| + | </p> | ||
| + | |||
| + | <h3>Scene List for the OspA:LA-2 Complex</h3> | ||
| + | <ul> | ||
| + | <li><scene name='Studio:G2SecL03/Ospafab-orig/3' target="complex">Reset model</scene><br><br></li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospafab-fab/3' target="complex">LA-2</scene> Fab antibody (Bluish regions indicate heavy chains (chains B & D of 1FJ1) and greenish regions indicate light chains (chains A & C of 1FJ1))</li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospafab-ospa/3' target="complex">OspA</scene> proteins in complex with the LA-2 Fab antibody (chains E & F of 1FJ1)</li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospafab-interaction/3' target="complex">Closeup</scene> of the OspA antigen : LA-2 Fab antibody interactions</li> | ||
| + | </ul> | ||
| + | |||
| + | |||
| + | |||
| + | <br><br><br><br> | ||
| + | |||
| + | <h2>Structure of OspA</h2> | ||
| + | |||
| + | <Structure load="1fj1" size="350" frame="true" align="right" name="OspA-manip" caption="Outer surface protein A (OspA) ([[1fj1|1FJ1]], chain F)" scene="Studio:G2SecL03/Ospa_3loopscartoon/3"/> | ||
| + | |||
| + | <p> | ||
| + | OspA is made up of 273 residues over 21 anti-parallel β-sheets and a single α-helix. It's folded conformation is divided into three main sections: a N-terminus "sandwich," a central region comprising of several β-sheets and a C-terminus "barrel" domain.<ref name="ding">PMID: 11183781</ref> The folded regions at its ends are connected by a single β-sheet layer in the middle, giving the protein the unique shape of a dumbell.<ref name="makabe">PMID: 16823038</ref> | ||
| + | |||
| + | There are <scene name='Studio:G2SecL03/Ospa-3loops/4' target="OspA-manip">three loops</scene> at the C-terminus of OspA that are important in binding with the LA-2 Fab antibody, whose interactions provide great insight into vaccine research and effectiveness. These three loops are linearly arranged and form protruding ridge at the C-terminus of OspA. Within these loops, there are <scene name='Studio:G2SecL03/Ospa-3residues-nor/3' target="OspA-manip">three residues</scene> <scene name='Studio:G2SecL03/Ospa-3residues-r/2' target="OspA-manip">(show residue R-groups)</scene> where there are distinct variations between the different strains of <i>Borrelia</i> and serve as potential targets for the creation of a broader vaccine.<ref name="ding">PMID: 11183781</ref> <scene name='Studio:G2SecL03/Ospa-3loops3res/1' target="OspA-manip">(display both the three loops and three residues together)</scene> | ||
| + | </p> | ||
| + | <p> | ||
| + | <scene name='Studio:G2SecL03/Ospa-loop1/1' target="OspA-manip">Loop 1</scene>, (residues 203-220), is important in showing variation amongst the different strains of <i>Borrelia</i> as well as being optimally conformed for binding without steric hindrance. <scene name='Studio:G2SecL03/Ospa-loop2/1' target="OspA-manip">Loop 2</scene> (residues 224-233) and <scene name='Studio:G2SecL03/Ospa-loop3/1' target="OspA-manip">Loop 3</scene> (residues 246-257) are more strongly conserved than Loop 1 but also help to show some variation amongst strains. The LA-2 Fab antibody readily recognizes OspA from <i>B. burgdorferi</i>, but does not recognize that from <i>B. afzelii</i> or <i>B. garinii</i>. | ||
| + | |||
| + | Between <i>B. burgdorferi</i> and <i>B. afzelii</i> genetic sequences are generally invariant, but two residues change between the species: <scene name='Studio:G2SecL03/Ospa-ala208/1' target="OspA-manip">Alanine (Ala) 208</scene> in <i>B. burgdorferi</i> is a Glutamine (Gln) in <i>B. afzelii</i>, and <scene name='Studio:G2SecL03/Ospa-asn251/1' target="OspA-manip">Asparagine (Asn) 251</scene> in <i>B. burgdorferi</i> is an Alanine (Ala) in <i>B. afzelii</i>. <i>B. garinii</i> has more variation and in addition to the previous two differences, having at least one more difference, where <scene name='Studio:G2SecL03/Ospa-ala215/1' target="OspA-manip">Alanine (Ala) 215</scene> in <i>B. burgdorferi</i> is a Lysine (Lys), and sometimes also has a deletion at <i>B. burgdorferi</i>’s Alanine 208. LA-2 and OspA of <i>B. burgdorferi</i> form a tight interface when binding, and the longer Glutamine (Gln) sidechain found in <i>B. afzelii</i> and <i>B. garinii</i> is more difficult to accommodate, causing less binding. A chimera that was weakly recognized by LA-2 was made with parts of loop 1 from <i>B. burgdorferi</i>, and loops 2 and 3 from <i>B. garinii</i>.<ref name="ding">PMID: 11183781</ref> Recently, a different kind of chimera has been made which combined the proximal region of <i>B. burgdorferi</i> and distal region of <i>B. afzelii</i>, and was able to successfully protect mice from both species.<ref name="livey">PMID: 21217174</ref> | ||
| + | </p> | ||
| + | |||
| + | |||
| + | <h3>Scene List for OspA</h3> | ||
| + | <ul> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa_3loopscartoon/3' target="OspA-manip">Reset model</scene><br><br></li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-3loops/4' target="OspA-manip">Three loops</scene> in C-terminus (close up) | ||
| + | <ul> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-loop1/1' target="OspA-manip">Loop 1</scene> (residues 203-220)</li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-loop2/1' target="OspA-manip">Loop 2</scene> (residues 224-233)</li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-loop3/1' target="OspA-manip">Loop 3</scene> (residues 246-257)</li> | ||
| + | </ul> | ||
| + | </li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-3residues-nor/3' target="OspA-manip">Three residues</scene> in C-terminus (Ala208, Ala215 and Asn251 in <i>B. burgdorferi</i>; also hides R-groups) | ||
| + | <ul> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-3residues-r/2' target="OspA-manip">Display R-groups</scene> of Ala208, Ala215 and Asn251</li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-ala208/1' target="OspA-manip">Alanine (Ala) 208</scene></li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-ala215/1' target="OspA-manip">Alanine (Ala) 215</scene></li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-asn251/1' target="OspA-manip">Asparagine (Asn) 251</scene></li> | ||
| + | </ul> | ||
| + | </li> | ||
| + | <li><scene name='Studio:G2SecL03/Ospa-3loops3res/1' target="OspA-manip">Three loops and all three residues (with R-groups included)</scene></li> | ||
| + | </ul> | ||
| + | |||
| + | |||
| + | |||
| + | <h2>References</h2> | ||
| + | <references /> | ||
| + | |||
| + | |||
| + | <h2>External Links</h2> | ||
| + | <ul> | ||
| + | <li>[http://www.who.int/ith/diseases/lyme/en/index.html World Health Organization: Lyme Disease] | ||
| + | <li>[http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002296/ PubMed Health: Lyme Disease] | ||
| + | <li>[http://www.aldf.com/ American Lyme Disease Foundation] | ||
| + | </ul> | ||
| + | |||
| + | |||
| + | <h2>Proteopedia Page Contributors and Editors</h2> | ||
| + | [http://proteopedia.org/wiki/index.php/User:Kimberly_Slade Kimberly Slade], [http://proteopedia.org/wiki/index.php/User:Cara_Lin Cara Lin], [http://proteopedia.org/wiki/index.php/User:Andrea_Mullen Andrea Mullen], [http://proteopedia.org/wiki/index.php/User:Jenny_Kim_Kim Jenny Kim Kim] | ||
| + | <br><br><br><br><br> | ||
Current revision
|
Outer Surface Protein A (OspA) is a major lipoprotein found on the surface of spirochetes from the genus Borrelia and is comprised of 21 anti-parallel β-sheets and a single α-helix. OspA's expression is regulated at different points in time, from being downregulated during the tick's feeding process on its host to being upregulated in the host's cerebrospinal fluid (CSF) to induce inflammatory response, resulting in acute Lyme neuroborreliosis. OspA has also been used as a vector in working towards the development of a vaccine for Lyme disease.
Contents |
Introduction
Lyme disease is caused by the spirochete Borrelia and spread via hard-bodied ticks belonging to the family Ixodidae. The Borrelia spirochetes are motile, helical organisms have several lipoproteins exposed on the surfaces of their membranes that invoke a response from host immune systems. The predominant group of these is classified as the outer surface proteins (Osps). Both the pathogenesis of Lyme disease as well as the host's immune response stem from the effects of the spirochete's presence and involvement in the system.[1] The major strain of Borrelia in the United States is Borrelia burgdorferi sensu stricto (Bb.), with 20-100 cases of Lyme disease being reported per 100,000 people. In Europe, Lyme disease cases are more prevalent, with 100-130 diagnoses per 100,000 people, but are caused by the spirochetes Borrelia afzelii (Ba.) and Borrelia garinii (Bg.) in addition to B. burgdorferi.[2][3]
Lyme disease is a debilitating condition that begins with a characteristic bullseye rash known as an erythema migrans (EM) as well as the development of lesions on other parts of the body, not just at the site of the tick's attachment to its host. Secondary stage symptoms include affecting the heart, joints, and both the central and peripheral nervous systems. OspA is used in adhering to the tick's gut by binding with the tick receptor for OspA (TROSPA), a receptor necessary for the colonization of Borrelia inside the tick. High levels of both OspA and TROSPA are found prior to feeding, but are downregulated once the feeding process begins in order to initiate transmission into the host.[4]
While feeding, OspA is downregulated in order to evade an immune response from the incoming host blood into the gut, releasing the Borrelia from the gut wall and migrating into the tick's salivary glands, thereby allowing it to enter the host through the bite. This is evidenced by the fact that patients with Lyme disease have been found to not possess OspA antibodies in the early stages of the disease.[1][2] OspA is the protein most related to acute Lyme neuroborreliosis (LNB), the neurological manifestations of Lyme disease.
OspA's Role in Invasion
Once inside the host, the Borrelia has a great number of mechanisms available to actively suppress the host's immune system response and neutralize its effector mechanisms, such as the expression of another outer surface protein, OspC, which prevents susceptibility to the host's innate immunity and complement systems. Additionally, Borrelia is capable of suppressing many of its surface proteins to reduce its detectability, but can also utilize protective means by temporarily expressing them when needed.
Acute Lyme Neuroborreliosis (LNB)
Acute Lyme Neuroborreliosis (LNB) is part of the second stage of Lyme disease in which the spirochete invades the peripheral and central nervous systems (CNS). Symptoms of LNB include: meningoradiculitis with inflammation of the nerve roots and radiculitis (Bannwarth’s syndrome), lymphocytic meningitis, and cranial and peripheral neuritis. In Europe, the strain predominantly found in the CSF of patients with Bannwarth's syndrome is B. garinii. However, in the United States, Bannwarth's syndrome is rare and the most common manifestations of Lyme neuroborreliosis is meningitis, caused by B. burgdorferi. The presence of OspA in the cerebrospinal fluid (CSF) is responsible for this complex inflammatory response in the brain that leads to the neuroborreliosis.[2]
Evasion and the Extracellular Matrix
The Borrelia are able to hide in the extracellular matrix, allowing it to survive by avoiding leukocytes circulating in the bloodstream. OspA can rapidly bind to plasminogen, which becomes plasmin once activated, and degrades the extracellular matrix. By binding to plasminogen, Borrelia could be exploiting its function and utilizing it to invade the extracellular matrix. However, due to the fact that OspA is downregulated during feeding, and stays unexpressed, a different mechanism may be used instead. Additionally, Borrelia induces the local upregulation of matrix metalloproteinase-9, causing the digestion of the surrounding extracellular matrix. Borrelia can also bind to several proteins in the extracellular matrix, such as fibronectin, integrins or decorin, which can aid in the spread and survival of the spirochetes in these tissues.[2]
Migration Across the Blood-Brain Barrier
It is not fully understood how Borrelia get past the blood-brain barrier, though some researchers suggest a paracellular route, which involves a process using transient tether-type associations, short-term dragging interactions, and stationary adhesion. There is evidence that Borrelia utilizes OspA in the transient tethering stage. The blood-brain barrier is composed of brain microvascular endothelial cells, astrocytes, a basement membrane, pericytes, and neurons. OspA is a major adherent molecule to brain microvascular cells by binding to the CD40 receptors outside, which results in events that are typically seen when leukocytes cross the blood brain barrier. Activation of CD40 receptors leads to the production of proinflammatory cytokines and enhanced expression of ICAM-1, E-selectin and VCAM-1, resulting in increased cell binding, and the formation of fenestrations due to increased vascular endothelial growth factor, and vascular permeability factor. OspA might be mimicking leukocytes in order to cross the blood-brain barrier. However not all strains of Borrelia can utilize OspA to do this, OspA only contributes about 70% to adherence, and other Borrelia proteins are also needed in this process. It has also been seen that OspA mediates the adhesion of Borrelia to murine neural and glial cell lines. [5]
Role in Inflammation
There are six steps involved in the host's inflammatory response to OspA: [2]
- When the Borrelia enter the host’s CNS they encounter several different types of immune cells such as monocytes, macrophages, and dendritic cells. While in the CSF, outer surface protein A (OspA) is upregulated and it’s increased expression promotes recognition by a specific receptor on a monocyte.
- The OspA-bound monocyte then releases proinflammatory cytokines (i.e. interferon), as well as chemokines, such as CXCL13. In patients with LNB, there is an observed increase in the levels of these cytokines and chemokines in their CSF. The production of chemokines leads to the recruitment of other immune cells to the site of infection.
- B-lymphocytes respond to the new concentration gradient of CXCL13 between the blood and CSF and migrate into the CSF.
- B-lymphocytes undergo receptor-mediated endocytosis, consuming the OspA antigens present in the CSF, thereby triggering its activation. The B-lymphocytes then are able to differentiate and mature into plasma cells.
- The plasma cells create large quantities of anti-OspA antibodies specific to this strain of Borrelia and release them into the CSF.
- The anti-OspA antibodies will then bind to the OspA on the spirochete’s membrane, thus killing the Borrelia.
This process is two-sided in the sense that the OspA aids in the pathogenesis of new symptoms (neuroborreliosis) through the chemokine’s actions, as well as initiating the signaling cascade to destroy itself.
OspA Vaccination
|
Risk of developing Lyme disease can be mitigated by staying clear of areas with populations of ticks, wearing proper attire to minimize easily bitten areas of the body, and using insect repellents containing DEET (N,N-diethy-m-toluamide). However, another effective means for prevention could be possible by using an outer surface protein from Borrelia in the creation of a vaccine.[6]
The membrane composition of Borrelia is abundant in both OspA and OspB, and the two proteins share a 53% similarity in their primary sequences. Both OspA and OspB are expressed in the tick's gut and downregulated during feeding and aid in its survivability; however, OspA is overall less varied and reactive than OspB, which has greater variability.[7] The relatively conserved sequence of OspA thus lends itself better to study and application toward the development of a vaccine for a broader range of Borrelia strains in the treatment of Lyme disease than that of OspB. The first vaccine used a purified recombinant form of OspA and functioned in blocking transmission of the spirochetes expressing OspA from tick to host during feeding, killing them while still attached to the tick's gut.[1][8] The vaccine, Lymerix, had shown 76% and 92% effectiveness in separate clinical trials in which patients were treated for two years following a three-dose schedule. However, the vaccination was suspended from use in 2002 when opponents claimed the IgG antibodies for OspA were associated with the onset of severe chronic arthritis, as well as other side effects affecting immunity.[1][9] This fact, in conjunction with the desire for a more widespread vaccine treating multiple strains of Borrelia, has spurred research towards a new vaccine.
To address the concerns of vaccine with broader protection, creation of a chimera, mixing the OspA of different strains of Borrelia would be ideal. Study of the epitope of and its with the murine monoclonal antibody have proved useful in determining effectiveness of a given vaccine trial as high levels of antibodies in test sera compete against LA-2 for binding with OspA. LA-2 makes direct contact with three exposed loops of the C-terminus of OspA. The recognition of OspA by LA-2 requires an induced fit mechanism where these three loops undergo conformational changes to optimize their interaction in the complex. [3]
Scene List for the OspA:LA-2 Complex
- Fab antibody (Bluish regions indicate heavy chains (chains B & D of 1FJ1) and greenish regions indicate light chains (chains A & C of 1FJ1))
- proteins in complex with the LA-2 Fab antibody (chains E & F of 1FJ1)
- of the OspA antigen : LA-2 Fab antibody interactions
Structure of OspA
|
OspA is made up of 273 residues over 21 anti-parallel β-sheets and a single α-helix. It's folded conformation is divided into three main sections: a N-terminus "sandwich," a central region comprising of several β-sheets and a C-terminus "barrel" domain.[3] The folded regions at its ends are connected by a single β-sheet layer in the middle, giving the protein the unique shape of a dumbell.[10] There are at the C-terminus of OspA that are important in binding with the LA-2 Fab antibody, whose interactions provide great insight into vaccine research and effectiveness. These three loops are linearly arranged and form protruding ridge at the C-terminus of OspA. Within these loops, there are where there are distinct variations between the different strains of Borrelia and serve as potential targets for the creation of a broader vaccine.[3]
, (residues 203-220), is important in showing variation amongst the different strains of Borrelia as well as being optimally conformed for binding without steric hindrance. (residues 224-233) and (residues 246-257) are more strongly conserved than Loop 1 but also help to show some variation amongst strains. The LA-2 Fab antibody readily recognizes OspA from B. burgdorferi, but does not recognize that from B. afzelii or B. garinii. Between B. burgdorferi and B. afzelii genetic sequences are generally invariant, but two residues change between the species: in B. burgdorferi is a Glutamine (Gln) in B. afzelii, and in B. burgdorferi is an Alanine (Ala) in B. afzelii. B. garinii has more variation and in addition to the previous two differences, having at least one more difference, where in B. burgdorferi is a Lysine (Lys), and sometimes also has a deletion at B. burgdorferi’s Alanine 208. LA-2 and OspA of B. burgdorferi form a tight interface when binding, and the longer Glutamine (Gln) sidechain found in B. afzelii and B. garinii is more difficult to accommodate, causing less binding. A chimera that was weakly recognized by LA-2 was made with parts of loop 1 from B. burgdorferi, and loops 2 and 3 from B. garinii.[3] Recently, a different kind of chimera has been made which combined the proximal region of B. burgdorferi and distal region of B. afzelii, and was able to successfully protect mice from both species.[11]
Scene List for OspA
- in C-terminus (close up)
- (residues 203-220)
- (residues 224-233)
- (residues 246-257)
- in C-terminus (Ala208, Ala215 and Asn251 in B. burgdorferi; also hides R-groups)
- of Ala208, Ala215 and Asn251
References
- ↑ 1.0 1.1 1.2 1.3 Connolly SE, Benach JL. The versatile roles of antibodies in Borrelia infections. Nat Rev Microbiol. 2005 May;3(5):411-20. PMID:15864264 doi:10.1038/nrmicro1149
- ↑ 2.0 2.1 2.2 2.3 2.4 Rupprecht TA, Koedel U, Fingerle V, Pfister HW. The pathogenesis of lyme neuroborreliosis: from infection to inflammation. Mol Med. 2008 Mar-Apr;14(3-4):205-12. PMID:18097481 doi:10.2119/2007-00091.Rupprecht
- ↑ 3.0 3.1 3.2 3.3 3.4 Ding W, Huang X, Yang X, Dunn JJ, Luft BJ, Koide S, Lawson CL. Structural identification of a key protective B-cell epitope in Lyme disease antigen OspA. J Mol Biol. 2000 Oct 6;302(5):1153-64. PMID:11183781 doi:10.1006/jmbi.2000.4119
- ↑ Pal U, Li X, Wang T, Montgomery RR, Ramamoorthi N, Desilva AM, Bao F, Yang X, Pypaert M, Pradhan D, Kantor FS, Telford S, Anderson JF, Fikrig E. TROSPA, an Ixodes scapularis receptor for Borrelia burgdorferi. Cell. 2004 Nov 12;119(4):457-68. PMID:15537536 doi:10.1016/j.cell.2004.10.027
- ↑ Pulzova L, Kovac A, Mucha R, Mlynarcik P, Bencurova E, Madar M, Novak M, Bhide M. OspA-CD40 dyad: ligand-receptor interaction in the translocation of neuroinvasive Borrelia across the blood-brain barrier. Sci Rep. 2011;1:86. Epub 2011 Sep 8. PMID:22355605 doi:10.1038/srep00086
- ↑ Nigrovic LE, Thompson KM. The Lyme vaccine: a cautionary tale. Epidemiol Infect. 2007 Jan;135(1):1-8. Epub 2006 Aug 8. PMID:16893489 doi:10.1017/S0950268806007096
- ↑ Becker M, Bunikis J, Lade BD, Dunn JJ, Barbour AG, Lawson CL. Structural investigation of Borrelia burgdorferi OspB, a bactericidal Fab target. J Biol Chem. 2005 Apr 29;280(17):17363-70. Epub 2005 Feb 15. PMID:15713683 doi:10.1074/jbc.M412842200
- ↑ Battisti JM, Bono JL, Rosa PA, Schrumpf ME, Schwan TG, Policastro PF. Outer surface protein A protects Lyme disease spirochetes from acquired host immunity in the tick vector. Infect Immun. 2008 Nov;76(11):5228-37. Epub 2008 Sep 8. PMID:18779341 doi:10.1128/IAI.00410-08
- ↑ Plotkin SA. Correcting a public health fiasco: The need for a new vaccine against Lyme disease. Clin Infect Dis. 2011 Feb;52 Suppl 3:s271-5. PMID:21217175 doi:10.1093/cid/ciq119
- ↑ Makabe K, Tereshko V, Gawlak G, Yan S, Koide S. Atomic-resolution crystal structure of Borrelia burgdorferi outer surface protein A via surface engineering. Protein Sci. 2006 Aug;15(8):1907-14. Epub 2006 Jul 5. PMID:16823038 doi:10.1110/ps.062246706
- ↑ Livey I, O'Rourke M, Traweger A, Savidis-Dacho H, Crowe BA, Barrett PN, Yang X, Dunn JJ, Luft BJ. A new approach to a Lyme disease vaccine. Clin Infect Dis. 2011 Feb;52 Suppl 3:s266-70. PMID:21217174 doi:10.1093/cid/ciq118
External Links
- World Health Organization: Lyme Disease
- PubMed Health: Lyme Disease
- American Lyme Disease Foundation
Proteopedia Page Contributors and Editors
Kimberly Slade, Cara Lin, Andrea Mullen, Jenny Kim Kim