Sandbox Reserved 1709
From Proteopedia
(Difference between revisions)
| (5 intermediate revisions not shown.) | |||
| Line 1: | Line 1: | ||
| - | + | =Vitamin K Epoxide Reductase= | |
<StructureSection load='VKORKO.pdb' size='340' side='right' caption='VKOR with KO bound.' scene='90/904314/Vkor_with_ko/2'> | <StructureSection load='VKORKO.pdb' size='340' side='right' caption='VKOR with KO bound.' scene='90/904314/Vkor_with_ko/2'> | ||
== Introduction== | == Introduction== | ||
=== Biological Role === | === Biological Role === | ||
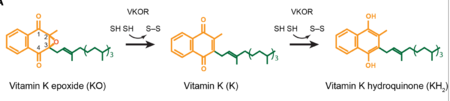
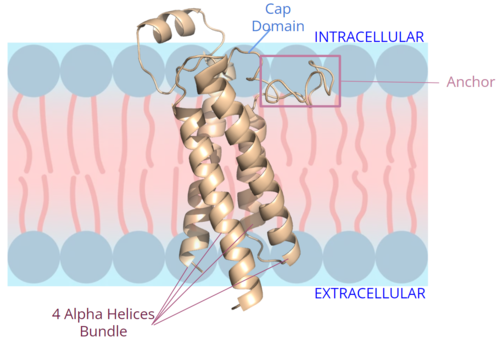
| - | <scene name='90/904314/Vkor_structure/1'>Vitamin K Epoxide Reductase</scene> (VKOR) is a reducing enzyme composed of 4-helices that spans the endoplasmic reticulum as a transmembrane protein<ref>DOI 10.1126/science.abc5667</ref>. Its enzymatic role is reducing <scene name='90/904314/Vkor_with_ko/7'>vitamin K epoxide</scene> (KO) to Vitamin K Hydroquinone (KH2)<ref>DOI 10.1021/bi700527j</ref> (Figure 1). The mechanism first occurs through the binding of KO and using two cysteine residues to reduce KO into [https://en.wikipedia.org/wiki/Vitamin_K Vitamin K]. Then, a second pair of cysteine residues will reduce Vitamin K into the final product, KH2 (Figure 1). One of VKOR's primary roles is to assist in blood coagulation through this KH2 regeneration mechanism.[[Image:VKOR_mechanism_2D.png|450 px|right|thumb|Figure 1. Mechanism of KO reduction into KH2.]] With Vitamin K as a cofactor, the [https://en.wikipedia.org/wiki/Gamma-glutamyl_carboxylase γ-carboxylase] enzyme will enact post-translational modification on KH2, oxidizing it back to KO <ref>DOI 10.1074/jbc.RA120.015401</ref>. The oxidation of KH2 by γ-carboxylase is coupled with the carboxylation of a glutamate residue to form γ-carboxyglutamate. The coupling of this oxidation and carboxylation will activate several clotting factors in the coagulation cascade. | + | <scene name='90/904314/Vkor_structure/1'>Vitamin K Epoxide Reductase</scene> (VKOR) is a reducing enzyme composed of 4-helices that spans the endoplasmic reticulum as a transmembrane protein<ref>DOI 10.1126/science.abc5667</ref>. Its enzymatic role is reducing <scene name='90/904314/Vkor_with_ko/7'>vitamin K epoxide</scene> (KO) to Vitamin K Hydroquinone (KH2)<ref>DOI 10.1021/bi700527j</ref> (Figure 1). The mechanism first occurs through the binding of KO and using two cysteine residues to reduce KO into [https://en.wikipedia.org/wiki/Vitamin_K Vitamin K]. Then, a second pair of cysteine residues will reduce Vitamin K into the final product, KH2 (Figure 1). One of VKOR's primary roles is to assist in blood coagulation through this KH2 regeneration mechanism.[[Image:VKOR_mechanism_2D.png|450 px|right|thumb|Figure 1. Mechanism of KO reduction into KH2<ref>DOI 10.1126/science.abc5667</ref>.]] With Vitamin K as a cofactor, the [https://en.wikipedia.org/wiki/Gamma-glutamyl_carboxylase γ-carboxylase] enzyme will enact post-translational modification on KH2, oxidizing it back to KO <ref>DOI 10.1074/jbc.RA120.015401</ref>. The oxidation of KH2 by γ-carboxylase is coupled with the carboxylation of a glutamate residue to form γ-carboxyglutamate. The coupling of this oxidation and carboxylation will activate several clotting factors in the coagulation cascade. |
=== Author's Notes === | === Author's Notes === | ||
| Line 29: | Line 29: | ||
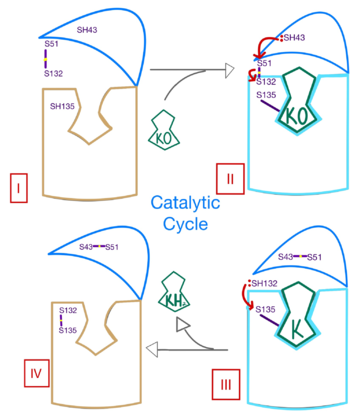
[[Image:Ss_of_catalytic_mech.png|350 px| right| thumb | Figure 3. Mechanism of VKOR.]] | [[Image:Ss_of_catalytic_mech.png|350 px| right| thumb | Figure 3. Mechanism of VKOR.]] | ||
| - | The catalytic mechanism of VKOR is highly regulated and uses <scene name='90/904314/Stage_4_catalytic_cycle/30'>4 catalytic cysteine residues</scene> to activate Vitamin K necessary for blood coagulation. Figure 3 highlights these reactions that allow the substrate to be catalyzed to its active form through a series of 4 stages. The enzyme begins in <scene name='90/904314/Vkor_with_ko/1'>stage I</scene> in the open conformation with the cap domain open to allow substrate binding. Once a substrate binds, the cap domain transitions to the closed conformation, initiating <scene name='90/904314/Stage_2_catalytic_cycle/ | + | The catalytic mechanism of VKOR is highly regulated and uses <scene name='90/904314/Stage_4_catalytic_cycle/30'>4 catalytic cysteine residues</scene> to activate Vitamin K necessary for blood coagulation. Figure 3 highlights these reactions that allow the substrate to be catalyzed to its active form through a series of 4 stages. The enzyme begins in <scene name='90/904314/Vkor_with_ko/1'>stage I</scene> in the open conformation with the cap domain open to allow substrate binding. Once a substrate binds, the cap domain transitions to the closed conformation, initiating <scene name='90/904314/Stage_2_catalytic_cycle/3'>stage II</scene>. For this to occur, the C51-C132 disulfide bridge is attacked by reactive C43 located within the cap domain. This reaction forms a new disulfide bridge between C43 and C51 that pulls the cap domain over the binding pocket with the substrate bound to stabilize the closed conformation of VKOR, such that VKOR is now in stage II. Free cysteines are now available that provide strong stabilization of the closed conformation through interactions with the cap domain and the bound substrate. This puts the enzyme in <scene name='90/904314/Stage_3_catalytic_cycle/8'>stage III</scene>, where a free C135 is purposed to interact with the substrate within the binding pocket to stabilize it during activation. The catalytic free C132 located between the cap domain and helical tunnel is very reactive and will attack this C135 to break that interaction with the substrate and release the activated Vitamin K product into the blood stream to promote coagulation. Two very stable disulfide bridges between C43-C41 and C132-C135 are now present and VKOR is unbound, so the enzyme is in its final, unreactive <scene name='90/904314/Stage_4_catalytic_cycle/21'>stage IV</scene>. VKOR must undergo conformational changes to return to Stage 1 and reactivate its catalytic cysteines so that another molecule of Vitamin K can bind and become activated. |
== Disease and Treatment == | == Disease and Treatment == | ||
| Line 37: | Line 37: | ||
=== Inhibition === | === Inhibition === | ||
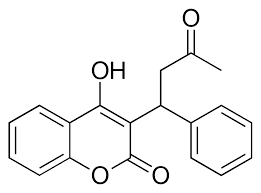
[[Image:Warfarin.png |400 px| right| thumb | Figure 4. Structure of Warfarin.]] | [[Image:Warfarin.png |400 px| right| thumb | Figure 4. Structure of Warfarin.]] | ||
| - | The most common way to treat blood clotting is using the VKOR inhibitor, <scene name='90/904314/Vkor_with_warfarin_bound/ | + | The most common way to treat blood clotting is using the VKOR inhibitor, <scene name='90/904314/Vkor_with_warfarin_bound/6'>warfarin</scene>. [https://en.wikipedia.org/wiki/Warfarin Warfarin] outcompetes KO<ref>PMID: 29261922</ref>, such that Vitamin K cannot be activated to promote coagulation in the blood. Warfarin will enter the binding pocket of VKOR, creating strong <scene name='90/906893/Vkor_with_warfarin_bound/3'>hydrogen bonds</scene> with the active site residues, N80 and Y139. Mutations of VKOR can lead to warfarin resistance which decreases its anticoagulation effects. Different mutations introduce varying degrees of resistance. These mutations are important to recognize as [https://en.wikipedia.org/wiki/Superwarfarin super-warfarin's] can be overly effective in anticoagulation and lead to fatality. |
=== Mutations === | === Mutations === | ||
| - | Mutations of the <scene name='90/906893/Vkor_with_warfarin_bound/4'>active site residues</scene> can occur within the binding pocket of VKOR. These mutations can be detrimental to the VKOR structure and function<ref>DOI 10.1126/science.abc5667</ref>. Two of the most common mutations occur to residues N80 and Y139 mutating them to <scene name='90/906893/Active_site_mutations/3'>A80 and F139</scene>. The change in polarity of these mutations from polar to nonpolar will cause a decrease in recognition and stabilization due to the inability to provide hydrogen bonds. | + | Mutations of the <scene name='90/906893/Vkor_with_warfarin_bound/4'>active site residues</scene> can occur within the binding pocket of VKOR. These mutations can be detrimental to the VKOR structure and function<ref>DOI 10.1126/science.abc5667</ref>. Two of the most common mutations occur to residues N80 and Y139 mutating them to <scene name='90/906893/Active_site_mutations/3'>A80 and F139</scene>. The change in polarity of these mutations from polar to nonpolar will cause a decrease in recognition and stabilization due to the inability to provide hydrogen bonds to the substrate. |
</StructureSection> | </StructureSection> | ||
| - | + | ==Proteopedia Page Contributors and Editors== | |
| + | Dr. Jeremy Johnson, Dr. Valentine Klimkowski, George Papadeas, Anna Pressel | ||
== References == | == References == | ||
<references/> | <references/> | ||
Current revision
Vitamin K Epoxide Reductase
| |||||||||||
Proteopedia Page Contributors and Editors
Dr. Jeremy Johnson, Dr. Valentine Klimkowski, George Papadeas, Anna Pressel
References
- ↑ Liu S, Li S, Shen G, Sukumar N, Krezel AM, Li W. Structural basis of antagonizing the vitamin K catalytic cycle for anticoagulation. Science. 2020 Nov 5. pii: science.abc5667. doi: 10.1126/science.abc5667. PMID:33154105 doi:http://dx.doi.org/10.1126/science.abc5667
- ↑ Jin DY, Tie JK, Stafford DW. The conversion of vitamin K epoxide to vitamin K quinone and vitamin K quinone to vitamin K hydroquinone uses the same active site cysteines. Biochemistry. 2007 Jun 19;46(24):7279-83. doi: 10.1021/bi700527j. Epub 2007 May, 25. PMID:17523679 doi:http://dx.doi.org/10.1021/bi700527j
- ↑ Liu S, Li S, Shen G, Sukumar N, Krezel AM, Li W. Structural basis of antagonizing the vitamin K catalytic cycle for anticoagulation. Science. 2020 Nov 5. pii: science.abc5667. doi: 10.1126/science.abc5667. PMID:33154105 doi:http://dx.doi.org/10.1126/science.abc5667
- ↑ Shen G, Cui W, Cao Q, Gao M, Liu H, Su G, Gross ML, Li W. The catalytic mechanism of vitamin K epoxide reduction in a cellular environment. J Biol Chem. 2021 Jan-Jun;296:100145. doi: 10.1074/jbc.RA120.015401. Epub 2020, Dec 10. PMID:33273012 doi:http://dx.doi.org/10.1074/jbc.RA120.015401
- ↑ Liu S, Li S, Shen G, Sukumar N, Krezel AM, Li W. Structural basis of antagonizing the vitamin K catalytic cycle for anticoagulation. Science. 2020 Nov 5. pii: science.abc5667. doi: 10.1126/science.abc5667. PMID:33154105 doi:http://dx.doi.org/10.1126/science.abc5667
- ↑ Liu S, Li S, Shen G, Sukumar N, Krezel AM, Li W. Structural basis of antagonizing the vitamin K catalytic cycle for anticoagulation. Science. 2020 Nov 5. pii: science.abc5667. doi: 10.1126/science.abc5667. PMID:33154105 doi:http://dx.doi.org/10.1126/science.abc5667
- ↑ Shen G, Cui W, Cao Q, Gao M, Liu H, Su G, Gross ML, Li W. The catalytic mechanism of vitamin K epoxide reduction in a cellular environment. J Biol Chem. 2021 Jan-Jun;296:100145. doi: 10.1074/jbc.RA120.015401. Epub 2020, Dec 10. PMID:33273012 doi:http://dx.doi.org/10.1074/jbc.RA120.015401
- ↑ Wang Y, Zhang W, Zhang Y, Yang Y, Sun L, Hu S, Chen J, Zhang C, Zheng Y, Zhen Y, Sun K, Fu C, Yang T, Wang J, Sun J, Wu H, Glasgow WC, Hui R. VKORC1 haplotypes are associated with arterial vascular diseases (stroke, coronary heart disease, and aortic dissection). Circulation. 2006 Mar 28;113(12):1615-21. doi: 10.1161/CIRCULATIONAHA.105.580167., Epub 2006 Mar 20. PMID:16549638 doi:http://dx.doi.org/10.1161/CIRCULATIONAHA.105.580167
- ↑ Elshaikh AO, Shah L, Joy Mathew C, Lee R, Jose MT, Cancarevic I. Influence of Vitamin K on Bone Mineral Density and Osteoporosis. Cureus. 2020 Oct 5;12(10):e10816. doi: 10.7759/cureus.10816. PMID:33173624 doi:http://dx.doi.org/10.7759/cureus.10816
- ↑ Patel S, Singh R, Preuss CV, Patel N. Warfarin PMID:29261922
- ↑ Liu S, Li S, Shen G, Sukumar N, Krezel AM, Li W. Structural basis of antagonizing the vitamin K catalytic cycle for anticoagulation. Science. 2020 Nov 5. pii: science.abc5667. doi: 10.1126/science.abc5667. PMID:33154105 doi:http://dx.doi.org/10.1126/science.abc5667