Sandbox GGC6
From Proteopedia
| Line 1: | Line 1: | ||
'''==Fibrinogen alpha chain==''' | '''==Fibrinogen alpha chain==''' | ||
| - | <StructureSection load='3VEV' size='340' side='right' caption='Caption for this structure' scene=''> | ||
| - | This is a default text for your page '''Sandbox GGC6'''. Click above on '''edit this page''' to modify. Be careful with the < and > signs. | ||
| - | You may include any references to papers as in: the use of JSmol in Proteopedia <ref>DOI 10.1002/ijch.201300024</ref> or to the article describing Jmol <ref>PMID:21638687</ref> to the rescue. | ||
| - | < | + | Fibrinogen ( factor I) is a plasma glycoprotein in the liver, that is important for proper blood clot formication. Fibrinogen is also synthesized in hepatic tissues. |
| + | |||
| + | Fibrinogen is composed of three pairs of polypeptide chains: two alpha, two beta, and two gamma <ref>PMID: 28101869</ref> | ||
| + | |||
== Function == | == Function == | ||
protease thrombin cleaves fibrinogen into monomers. The formation of monomers, fibrinogen beta, and fibrinogen alpha is insoluble fibrin matrix. fibrin works as a binding or trapping agent in the coagulation process, which creates blood clot. | protease thrombin cleaves fibrinogen into monomers. The formation of monomers, fibrinogen beta, and fibrinogen alpha is insoluble fibrin matrix. fibrin works as a binding or trapping agent in the coagulation process, which creates blood clot. | ||
Revision as of 02:34, 16 November 2020
==Fibrinogen alpha chain==
Fibrinogen ( factor I) is a plasma glycoprotein in the liver, that is important for proper blood clot formication. Fibrinogen is also synthesized in hepatic tissues.
Fibrinogen is composed of three pairs of polypeptide chains: two alpha, two beta, and two gamma [1]
Contents |
Function
protease thrombin cleaves fibrinogen into monomers. The formation of monomers, fibrinogen beta, and fibrinogen alpha is insoluble fibrin matrix. fibrin works as a binding or trapping agent in the coagulation process, which creates blood clot.
For small wounds, the polymerized fibrin with platelets forms a hemostatic plug over the wounds site. Fibrin is also anti inflammatory which it protects against IFNG- mediated hemorrhage.
Afibrinogenemic pregnant patients will result in spontaneous miscarriage. Fibrinogen supplemental will allow the patients to sustain the pregnancy, therefore, maternal fibrinogen plays a important role for successful pregnancy.[2]
Disease
Congenital afibrinogenemia (CAFBN)
This is an inherited blood disorder where the blood does not clot normally. This disease is caused by truncating mutations. Changing in position Arg-35 when Thrombin cleaves the site of Fibrinopeptide leads to alpha- Dysfibrinogenemias. [3]
Nosebleeds, bleeding from the gums and tongue are commons after a minor trauma for people with this disease. bleedings in the brain and internal organs can occur for affected individuals which can lead to be fatal. However, it's rare. Women with this disease can experience an abnormal heavy menstrual bleeding, they could also have a difficult time carrying a pregnancy, and could result in miscarriages. Newborn with this disease can experience bleeding from the umbilical cord stump after birth. The treatment for this disease includes cryoprecipitate, fibrinogen, and plasma (contains clotting factors). [4]
Amyloidosis 8 (AMYL8)
This is hereditary disease which insoluble amyloid proteins deposits in body tissues and organs. This tends to abnormal protein build-up and leads to damaged organs and deaths. The disease is caused by a mutation fibrinogen alpha chain.[5] This disease does not show symptoms at first stage. when it gets relatively advanced, the symptoms can be lack of appetite, weight loss, fatigue, weakness, shortness of breath, etc. Due to abnormal protein build-up in body organs, organs can be affected such as heart, liver, kidney, skin, etc. This leads to cardiomyopathy, liver failure, skin rash, nephrotic syndrome. However, nervous system is not affected. There is no treatment for this disease [6].
Congenital Dysfibrinogenemia.
This is either inherited or acquired disorder caused by having abnormal form of fibrinogen. This leads to an abnormal blood clot formation; it could be increase or decrease ability to clot. Acquired dysfibrinogenemia is more common and associated with liver disease such as hepatitis, liver tumors. Most of people with this disease have no symptoms and do not need a treatment. [7]
Relevance
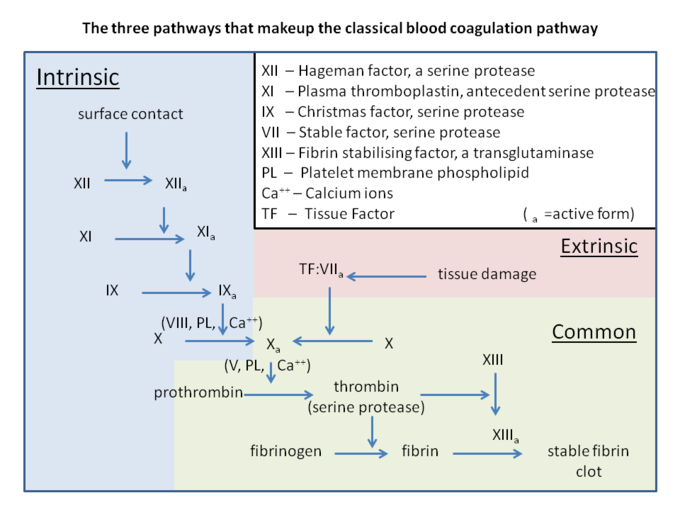
This process called coagulation cascade (or secondary hemostasis) forming a stable insoluble fibrin clot. The process has two pathways which are intrinsic and extrinsic pathway. These pathways eventually join to become the common pathway.
- Intrinsic pathway: This begins with activated factor XII, which then activates factor XI. Activated factor XI further activates factor IX, which activates factor VIII to form tenase complex on a phospholipid surface to activate factor X in the common pathway.
- Extrinsic pathway: when a tissue is damaged, it releases tissue factor to activate factor VII, which then activates factor X. - Common pathway:'' either intrinsic pathway or extrinsic pathway activates factor X causes formation of thrombin from prothrombin. Thrombin will cleave fibrinogen to insoluble fibrin and also activate factor XIII. Factor XIII and fibrin bind together forming a stable bond and attach to platelets. [8]
Structural highlights
</StructureSection>
References
- ↑ Weisel JW, Litvinov RI. Fibrin Formation, Structure and Properties. Subcell Biochem. 2017;82:405-456. doi: 10.1007/978-3-319-49674-0_13. PMID:28101869 doi:http://dx.doi.org/10.1007/978-3-319-49674-0_13
- ↑ Iwaki T, Castellino FJ. Maternal fibrinogen is necessary for embryonic development. Curr Drug Targets. 2005 Aug;6(5):535-9. doi: 10.2174/1389450054546006. PMID:16026273 doi:http://dx.doi.org/10.2174/1389450054546006
- ↑ Asselta R, Plate M, Robusto M, Borhany M, Guella I, Solda G, Afrasiabi A, Menegatti M, Shamsi T, Peyvandi F, Duga S. Clinical and molecular characterisation of 21 patients affected by quantitative fibrinogen deficiency. Thromb Haemost. 2015 Mar;113(3):567-76. doi: 10.1160/TH14-07-0629. Epub 2014 Nov , 27. PMID:25427968 doi:http://dx.doi.org/10.1160/TH14-07-0629
- ↑ de Moerloose P, Neerman-Arbez M. Congenital fibrinogen disorders. Semin Thromb Hemost. 2009 Jun;35(4):356-66. doi: 10.1055/s-0029-1225758. Epub, 2009 Jul 13. PMID:19598064 doi:http://dx.doi.org/10.1055/s-0029-1225758
- ↑ Baker KR, Rice L. The amyloidoses: clinical features, diagnosis and treatment. Methodist Debakey Cardiovasc J. 2012 Jul-Sep;8(3):3-7. doi: 10.14797/mdcj-8-3-3. PMID:23227278 doi:http://dx.doi.org/10.14797/mdcj-8-3-3
- ↑ Benson MD, Liepnieks J, Uemichi T, Wheeler G, Correa R. Hereditary renal amyloidosis associated with a mutant fibrinogen alpha-chain. Nat Genet. 1993 Mar;3(3):252-5. PMID:8097946 doi:http://dx.doi.org/10.1038/ng0393-252
- ↑ Casini A, Blondon M, Lebreton A, Koegel J, Tintillier V, de Maistre E, Gautier P, Biron C, Neerman-Arbez M, de Moerloose P. Natural history of patients with congenital dysfibrinogenemia. Blood. 2015 Jan 15;125(3):553-61. doi: 10.1182/blood-2014-06-582866. Epub 2014, Oct 15. PMID:25320241 doi:http://dx.doi.org/10.1182/blood-2014-06-582866
- ↑ Palta S, Saroa R, Palta A. Overview of the coagulation system. Indian J Anaesth. 2014 Sep;58(5):515-23. doi: 10.4103/0019-5049.144643. PMID:25535411 doi:http://dx.doi.org/10.4103/0019-5049.144643