We apologize for Proteopedia being slow to respond. For the past two years, a new implementation of Proteopedia has been being built. Soon, it will replace this 18-year old system. All existing content will be moved to the new system at a date that will be announced here.
Sandbox Reserved 1779
From Proteopedia
(Difference between revisions)
| Line 9: | Line 9: | ||
===Overview=== | ===Overview=== | ||
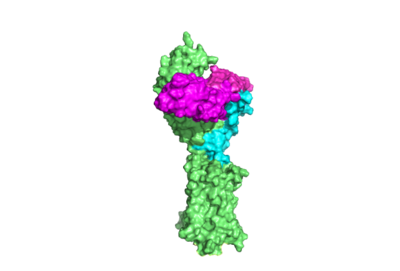
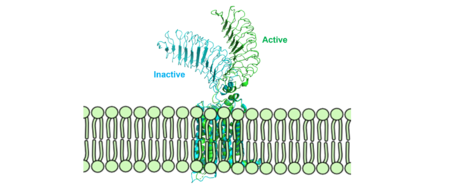
The thyrotropin receptor has an extracellular domain (ECD) that is composed of a <scene name='95/952709/Lrrd_real/2'>leucine rich repeat domain (LRRD)</scene> as well as a hinge region. This <scene name='95/952709/Hinge_region_real/2'>hinge region</scene> links the ECD to the seven transmembrane helices <scene name='95/952709/7tm_helices/4'>(7TM domain)</scene>, which span from the extracellular domain to the intracellular domain <ref name= "Keinau et al.">Kleinau, G., Worth, C. L., Kreuchwig, A., Biebermann, H., Marcinkowski, P., Scheerer, P., & Krause, G. (2017). Structural–functional features of the thyrotropin receptor: A class A G-protein-coupled receptor at work. Frontiers in Endocrinology, 8. https://doi.org/10.3389/fendo.2017.00086</ref>. Thyrotropin binding causes a conformational change in the ECD that is transduced through the transmembrane helices. In the active state, the ECD is in the "up" position, while in the inactive state, the ECD is in the "down" state, closer to the cell membrane. A "push-pull" mechanism is proposed to be responsible for the ECD's conformational change between active and inactive states. In the "push" model, TSH binds to the receptor and sterically clashes with the cellular membrane forcing the ECD up away from the membrane. In the pull model, a short α-helix interacts with TSH to pull the ECD up. The active (up) form of the ECD causes a conformation shift in the TMD which causes differential interactions with a heterotrimeric <scene name='95/952709/G_protein/2'>G-protein</scene>, initiating intracellular signaling<ref name="Duan et al.">PMID:35940204</ref>. | The thyrotropin receptor has an extracellular domain (ECD) that is composed of a <scene name='95/952709/Lrrd_real/2'>leucine rich repeat domain (LRRD)</scene> as well as a hinge region. This <scene name='95/952709/Hinge_region_real/2'>hinge region</scene> links the ECD to the seven transmembrane helices <scene name='95/952709/7tm_helices/4'>(7TM domain)</scene>, which span from the extracellular domain to the intracellular domain <ref name= "Keinau et al.">Kleinau, G., Worth, C. L., Kreuchwig, A., Biebermann, H., Marcinkowski, P., Scheerer, P., & Krause, G. (2017). Structural–functional features of the thyrotropin receptor: A class A G-protein-coupled receptor at work. Frontiers in Endocrinology, 8. https://doi.org/10.3389/fendo.2017.00086</ref>. Thyrotropin binding causes a conformational change in the ECD that is transduced through the transmembrane helices. In the active state, the ECD is in the "up" position, while in the inactive state, the ECD is in the "down" state, closer to the cell membrane. A "push-pull" mechanism is proposed to be responsible for the ECD's conformational change between active and inactive states. In the "push" model, TSH binds to the receptor and sterically clashes with the cellular membrane forcing the ECD up away from the membrane. In the pull model, a short α-helix interacts with TSH to pull the ECD up. The active (up) form of the ECD causes a conformation shift in the TMD which causes differential interactions with a heterotrimeric <scene name='95/952709/G_protein/2'>G-protein</scene>, initiating intracellular signaling<ref name="Duan et al.">PMID:35940204</ref>. | ||
| + | |||
=== Active and Inactive Form === | === Active and Inactive Form === | ||
| - | [[Image: | + | [[Image:Morphmembrane.png|450 px|right|thumb|Figure 2: Inactive form of the thyrotropin receptor shown in blue (PDB: 7T9M). Active form of the thyrotropin receptor shown in green (PDB: 7T9I).]] |
| - | The TSHR protein exists in two states: active and inactive (Figure 2) (GREEN LINK ?) | + | The TSHR protein exists in two states: active and inactive (Figure 2) (GREEN LINK ?). The <scene name='95/952708/Tshr_chainr/4'>TSHR active form</scene> (GREEN LINK take away extra molecules) exists in dynamic equilibrium where <scene name='95/952708/Tsh_7t9i/1'>TSH</scene> (GREEN LINK make TSH one color) binding favors the active state. In this active state, TSH will bind and keep the active state in the up position because of clashes between bound TSH and the cell membrane.<ref name="Faust" />. Glycosylations of the Asn52 residue cause this clash (GREEN LINK) on the <scene name='95/952707/Tsh_7t9i/1'>α-subunit of TSH</scene>. The addition of N-acetyl glucosamine modifications creates steric clashes between TSH and the cell membrane, keeping TSHR in the active state. |
| + | |||
=== Leucine Rich Repeats === | === Leucine Rich Repeats === | ||
The Leucine Rich Repeat Domain (LRRD) is part of the <scene name='95/952708/Tshr_chainr_ecd/1'>ECD</scene> of TSHR and contains <scene name='95/952707/Lrr/3'>10-11 Leucine Rich Repeats</scene>. A unique feature of this region is that it is composed entirely of β-pleated sheets. These β-pleated sheets of the LRRD provides a concave binding surface for TSH, including <scene name='95/952707/Interactions_with_thyrotropin/2'>K209 and K58</scene> <ref name="Duan et al.">PMID: 35940204</ref>. These interact with <scene name='95/952707/Interactions_with_thyrotropin/2'>N91 and E98</scene> in the seatbelt region of TSH forming a salt bridge and initiating the conformational change by pulling on the hinge region of the receptor <ref name="Faust">PMID: 35940205</ref>. This interaction is specific to TSH and TSHR. When other agonists or antagonists bind to the receptor, the change in conformation is a result of different residues interacting, as explained later in the page. The Leucine residues in the LRRD determine ECD folding and which residues are located on the exterior protein and interacting with ligands. | The Leucine Rich Repeat Domain (LRRD) is part of the <scene name='95/952708/Tshr_chainr_ecd/1'>ECD</scene> of TSHR and contains <scene name='95/952707/Lrr/3'>10-11 Leucine Rich Repeats</scene>. A unique feature of this region is that it is composed entirely of β-pleated sheets. These β-pleated sheets of the LRRD provides a concave binding surface for TSH, including <scene name='95/952707/Interactions_with_thyrotropin/2'>K209 and K58</scene> <ref name="Duan et al.">PMID: 35940204</ref>. These interact with <scene name='95/952707/Interactions_with_thyrotropin/2'>N91 and E98</scene> in the seatbelt region of TSH forming a salt bridge and initiating the conformational change by pulling on the hinge region of the receptor <ref name="Faust">PMID: 35940205</ref>. This interaction is specific to TSH and TSHR. When other agonists or antagonists bind to the receptor, the change in conformation is a result of different residues interacting, as explained later in the page. The Leucine residues in the LRRD determine ECD folding and which residues are located on the exterior protein and interacting with ligands. | ||
| Line 20: | Line 22: | ||
| - | == TSHR Agonists and Antagonists == | ||
| - | Chemical [https://en.wikipedia.org/wiki/Agonist agonists] are found in many living systems and serve as a way to activate receptors or pathways that are necessary for a wide array of biological processes. Chemical [https://en.wikipedia.org/wiki/Receptor_antagonist antagonists] block or inhibit biological processes. Different types of agonists/antagonists exist within the body including hormones, antibodies, and neurotransmitters. The body naturally produces autoantibodies that can act as agonists and mimic the activating mechanism of the natural hormone. Isolating these antibodies in patients with diseases can lead researchers to uncover the mechanism of binding for the receptor. | ||
| - | |||
| - | ===M22 Agonist and Grave's Disease=== | ||
| - | <scene name='95/952708/M22_edited/3'>M22</scene> is a [https://en.wikipedia.org/wiki/Monoclonal_antibody monoclonal antibody] that produced by patients with [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease Graves' Disease]. Grave's Disease is an autoimmune disease that is a result of hyperthyroidism, where too much TSH is being produced. This disease [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease effects 1 in 100 Americans and especially women or people older than 30 years of age]. The binding of <scene name='95/952708/Tsh_7t9i/1'>TSH</scene> to <scene name='95/952709/Initial_scene_with_edited_7utz/2'>TSHR</scene> results in the receptor remaining in its active conformation. In Graves' disease, autoantibodies mimic TSH function and cause thyroid overactivity. <ref name="Miguel"> doi:10.1677/JME-08-0152</ref>. The M22 [https://en.wikipedia.org/wiki/Autoantibody autoantibody] activates TSHR by causing a membrane clash with the ECD and cell membrane, keeping the TSHR in the active state by preventing the TSHR from rotating to the inactive state (Figure 3). M22 mimics TSH activation of TSHR, and is a potent activator for intracellular signaling. <ref name="Faust"> DOI:10.1038/s41586-022-05159-1</ref> Although M22 binds in a similar manner to TSH, M22 does not interact with the hinge region when bound to TSHR, whereas TSH bound to TSHR does.<ref name="Faust"> DOI:10.1038/s41586-022-05159-1</ref> This finding shows that the hinge region is not necessary for the activation of TSHR, and leads to the discovery of other methods of activation. [[Image:Agonist pic.png|450 px|right|thumb|Figure 3: Agonist and antagonist drugs for activating or inactivating the TSHR protein. Here the membrane clashes are demonstrated on TSHR with different agonists attached. CS-17 is orange, TSH is purple, and M22 is blue in the figure. The TSHR protein is green and embedded in the protein.]] | ||
| + | == TSHR Agonists and Antagonists == | ||
| + | Chemical [https://en.wikipedia.org/wiki/Agonist agonists] are found in many living systems and serve as a way to activate receptors or pathways that are necessary for a wide array of biological processes. Chemical [https://en.wikipedia.org/wiki/Receptor_antagonist antagonists] block or inhibit biological processes. Different types of agonists/antagonists exist within the body including hormones, antibodies, and neurotransmitters. The body naturally produces autoantibodies that can act as agonists and mimic the activating mechanism of the natural hormone.<ref name="Miguel"> doi:10.1677/JME-08-0152</ref>. | ||
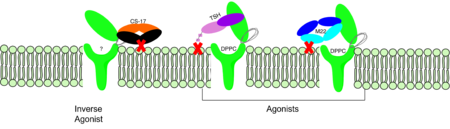
| + | ===M22 Agonist=== | ||
| + | <scene name='95/952708/M22_edited/3'>M22</scene> is a [https://en.wikipedia.org/wiki/Monoclonal_antibody monoclonal antibody] that is produced by patients with [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease Graves' Disease]. In Graves' disease, autoantibodies mimic TSH function and cause thyroid overactivity. <ref name="Miguel"> doi:10.1677/JME-08-0152</ref>. Grave's Disease is an autoimmune disease that is a result of hyperthyroidism, where too much TSH is being produced. This disease [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease effects 1 in 100 Americans and especially women or people older than 30 years of age]. The M22 [https://en.wikipedia.org/wiki/Autoantibody autoantibody] activates TSHR by causing a membrane clash with the ECD and cell membrane, keeping the TSHR in the active state by preventing the TSHR from rotating to the inactive state (Figure 3). M22 mimics TSH activation of TSHR, and is a potent activator for intracellular signaling. <ref name="Faust"> DOI:10.1038/s41586-022-05159-1</ref> Although M22 binds in a similar manner to TSH, M22 does not interact with the hinge region when bound to TSHR, whereas TSH bound to TSHR does.<ref name="Faust"> DOI:10.1038/s41586-022-05159-1</ref> This finding shows that the hinge region is not necessary for the activation of TSHR, and leads to the discovery of other methods of activation. [[Image:Agonist pic.png|450 px|right|thumb|Figure 3: Agonist and antagonist drugs for activating or inactivating the TSHR protein. Here the membrane clashes are demonstrated on TSHR with different agonists attached. CS-17 is orange, TSH is purple, and M22 is blue in the figure. The TSHR protein is green and embedded in the protein.]] | ||
===CS-17 Inverse Agonist=== | ===CS-17 Inverse Agonist=== | ||
| - | <scene name='95/952707/Cs17/3'>CS-17</scene> is a [https://en.wikipedia.org/wiki/Monoclonal_antibody monoclonal antibody] that acts as an inverse agonist for TSHR constitutive activity. <ref name= "Chen et al.">Chen, C.-R., McLachlan, S. M., & Rapoport, B. (2007). Suppression of thyrotropin receptor constitutive activity by a monoclonal antibody with inverse agonist activity. Endocrinology, 148(5), 2375–2382. https://doi.org/10.1210/en.2006-1754</ref>. An example of disease caused by inverse agonists is [https://www.mayoclinic.org/diseasesconditions/hypothyroidism/symptomscauses/syc20350284#:~:text=Hypothyroidism%20happens%20when%20the%20thyroid,symptoms%20in%20its%20early%20stages hypothyroidism]. The most common cause of hypothyroidism is [https://www.mayoclinic.org/diseasesconditions/hypothyroidism/symptomscauses/syc20350284#:~:text=Hypothyroidism%20happens%20when%20the%20thyroid,symptoms%20in%20its%20early%20stages Hashimoto’s disease]. Without enough TSH to bind TSHR, the pathway remains inactive and thus metabolic processes are inhibited in this pathway. CS-17 interacts with the ECD of the TSHR protein on the convex side GREEN LINK of the LRRD, suppressing TSHR function by keeping the receptor in the inactive state (Figure 3). Clash of bound CS-17 with the cell membrane locks TSHR in the inactive form. This type of inhibition is uncommon and is a promising mechanism for future drug design and research to combat hypothyroidism.<ref name="Chen et al.">Chen, C.-R., McLachlan, S. M., & Rapoport, B. (2007). Suppression of thyrotropin receptor constitutive activity by a monoclonal antibody with inverse agonist activity. Endocrinology, 148(5), 2375–2382. https://doi.org/10.1210/en.2006-1754</ref>. | + | <scene name='95/952707/Cs17/3'>CS-17</scene> (GREEN LINK add TMD and 1 color for CS-17) is a [https://en.wikipedia.org/wiki/Monoclonal_antibody monoclonal antibody] that acts as an inverse agonist for TSHR constitutive activity. <ref name= "Chen et al.">Chen, C.-R., McLachlan, S. M., & Rapoport, B. (2007). Suppression of thyrotropin receptor constitutive activity by a monoclonal antibody with inverse agonist activity. Endocrinology, 148(5), 2375–2382. https://doi.org/10.1210/en.2006-1754</ref>. An example of a disease caused by inverse agonists is [https://www.mayoclinic.org/diseasesconditions/hypothyroidism/symptomscauses/syc20350284#:~:text=Hypothyroidism%20happens%20when%20the%20thyroid,symptoms%20in%20its%20early%20stages hypothyroidism]. The most common cause of hypothyroidism is [https://www.mayoclinic.org/diseasesconditions/hypothyroidism/symptomscauses/syc20350284#:~:text=Hypothyroidism%20happens%20when%20the%20thyroid,symptoms%20in%20its%20early%20stages Hashimoto’s disease]. Without enough TSH to bind TSHR, the pathway remains inactive and thus metabolic processes are inhibited in this pathway. CS-17 interacts with the ECD of the TSHR protein on the convex side GREEN LINK of the LRRD, suppressing TSHR function by keeping the receptor in the inactive state (Figure 3). Clash of bound CS-17 with the cell membrane locks TSHR in the inactive form. This type of inhibition is uncommon and is a promising mechanism for future drug design and research to combat hypothyroidism.<ref name="Chen et al.">Chen, C.-R., McLachlan, S. M., & Rapoport, B. (2007). Suppression of thyrotropin receptor constitutive activity by a monoclonal antibody with inverse agonist activity. Endocrinology, 148(5), 2375–2382. https://doi.org/10.1210/en.2006-1754</ref>. |
| - | ===TSH Agonist=== | ||
| - | This clash is caused by glycosylations of an Asn52 on the <scene name='95/952707/Tsh_7t9i/1'>α-subunit of TSH</scene>. Addition of N-acetyl glucosamine modifications create steric clashes between TSH and the cell membrane, keeping TSHR in the active state. | ||
Revision as of 20:56, 12 April 2023
>
| This Sandbox is Reserved from February 27 through August 31, 2023 for use in the course CH462 Biochemistry II taught by R. Jeremy Johnson at the Butler University, Indianapolis, USA. This reservation includes Sandbox Reserved 1765 through Sandbox Reserved 1795. |
To get started:
More help: Help:Editing |
| |||||||||||
References
- ↑ 1.0 1.1 1.2 Yen PM. Physiological and molecular basis of thyroid hormone action. Physiol Rev. 2001 Jul;81(3):1097-142. doi: 10.1152/physrev.2001.81.3.1097. PMID: 11427693.
- ↑ Pirahanchi Y, Toro F, Jialal I. Physiology, Thyroid Stimulating Hormone. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499850/
- ↑ 3.0 3.1 3.2 3.3 Duan J, Xu P, Luan X, Ji Y, He X, Song N, Yuan Q, Jin Y, Cheng X, Jiang H, Zheng J, Zhang S, Jiang Y, Xu HE. Hormone- and antibody-mediated activation of the thyrotropin receptor. Nature. 2022 Aug 8. pii: 10.1038/s41586-022-05173-3. doi:, 10.1038/s41586-022-05173-3. PMID:35940204 doi:http://dx.doi.org/10.1038/s41586-022-05173-3
- ↑ Kohn LD, Shimura H, Shimura Y, Hidaka A, Giuliani C, Napolitano G, Ohmori M, Laglia G, Saji M. The thyrotropin receptor. Vitam Horm. 1995;50:287-384. doi: 10.1016/s0083-6729(08)60658-5. PMID: 7709602.
- ↑ 5.0 5.1 5.2 Kleinau, G., Worth, C. L., Kreuchwig, A., Biebermann, H., Marcinkowski, P., Scheerer, P., & Krause, G. (2017). Structural–functional features of the thyrotropin receptor: A class A G-protein-coupled receptor at work. Frontiers in Endocrinology, 8. https://doi.org/10.3389/fendo.2017.00086
- ↑ 6.0 6.1 6.2 6.3 Faust B, Billesbolle CB, Suomivuori CM, Singh I, Zhang K, Hoppe N, Pinto AFM, Diedrich JK, Muftuoglu Y, Szkudlinski MW, Saghatelian A, Dror RO, Cheng Y, Manglik A. Autoantibody mimicry of hormone action at the thyrotropin receptor. Nature. 2022 Aug 8. pii: 10.1038/s41586-022-05159-1. doi:, 10.1038/s41586-022-05159-1. PMID:35940205 doi:http://dx.doi.org/10.1038/s41586-022-05159-1
- ↑ Yumiko Mizutori, Chun-Rong Chen, Sandra M. McLachlan, Basil Rapoport, The Thyrotropin Receptor Hinge Region Is Not Simply a Scaffold for the Leucine-Rich Domain but Contributes to Ligand Binding and Signal Transduction, Molecular Endocrinology, Volume 22, Issue 5, 1 May 2008, Pages 1171–1182, https://doi.org/10.1210/me.2007-0407
- ↑ 8.0 8.1 8.2 8.3 Faust, B., Billesbølle, C.B., Suomivuori, CM. et al. Autoantibody mimicry of hormone action at the thyrotropin receptor. Nature 609, 846–853 (2022). https://doi.org/10.1038/s41586-022-
- ↑ Virginie Vlaeminck-Guillem, Su-Chin Ho, Patrice Rodien, Gilbert Vassart, Sabine Costagliola, Activation of the cAMP Pathway by the TSH Receptor Involves Switching of the Ectodomain from a Tethered Inverse Agonist to an Agonist, Molecular Endocrinology, Volume 16, Issue 4, 1 April 2002, Pages 736–746, https://doi.org/10.1210/mend.16.4.0816
- ↑ Goricanec, D., Stehle, R., Egloff, P., Grigoriu, S., Plückthun, A., Wagner, G., & Hagn, F. (2016). Conformational dynamics of a G-protein α subunit is tightly regulated by nucleotide binding. Proceedings of the National Academy of Sciences, 113(26). https://doi.org/10.1073/pnas.1604125113
- ↑ 11.0 11.1 Nunez Miguel R, Sanders J, Chirgadze DY, Furmaniak J, Rees Smith B. Thyroid stimulating autoantibody M22 mimics TSH binding to the TSH receptor leucine rich domain: a comparative structural study of protein-protein interactions. J Mol Endocrinol. 2009 May;42(5):381-95. Epub 2009 Feb 16. PMID:19221175 doi:10.1677/JME-08-0152
- ↑ 12.0 12.1 Chen, C.-R., McLachlan, S. M., & Rapoport, B. (2007). Suppression of thyrotropin receptor constitutive activity by a monoclonal antibody with inverse agonist activity. Endocrinology, 148(5), 2375–2382. https://doi.org/10.1210/en.2006-1754