This old version of Proteopedia is provided for student assignments while the new version is undergoing repairs. Content and edits done in this old version of Proteopedia after March 1, 2026 will eventually be lost when it is retired in about June of 2026.
Apply for new accounts at the new Proteopedia. Your logins will work in both the old and new versions.
User:Marvin O'Neal/OspA
From Proteopedia
| Line 67: | Line 67: | ||
<Structure load="1fj1" size="350" frame="true" align="right" name="OspA-manip" caption="Outer surface protein A (OspA) ([[1fj1|1FJ1]], chain F)" scene="Studio:G2SecL03/Ospa_3loopscartoon/3"/> | <Structure load="1fj1" size="350" frame="true" align="right" name="OspA-manip" caption="Outer surface protein A (OspA) ([[1fj1|1FJ1]], chain F)" scene="Studio:G2SecL03/Ospa_3loopscartoon/3"/> | ||
| - | |||
| - | <scene name='Studio:G2SecL03/Ospa_3loopscartoon/3' target="OspA-manip">Reset Model</scene> | ||
<p> | <p> | ||
Revision as of 00:16, 2 May 2012
|
Outer Surface Protein A (OspA) is a major lipoprotein found on the surface of spirochetes from the genus Borrelia, and is downregualted during the initial biting and feeding process of the tick. It is also involved in the manifestation of Lyme Neuroborreliosis. OspA was used to make the first vaccine for Lyme disease. is a major lipoprotein found on the surface of spirochetes from the genus Borrelia and is comprised of 21 anti-parallel β-strands and a single α-helix. OspA's expression is regulated at different points in time, from being downregulated during the tick's feeding process on its host to being upregulated in the host's cerebrospinal fluid (CSF) to induce inflammatory response, resulting in acute Lyme neuroborreliosis. OspA has also been used as a vector in working towards the development of a vaccine for Lyme disease.
NOTE: Red text indicates changes/additions I've made and this style is pertinent thoughts/questions we should consider/address. All of this will be cleaned up for the final submitted page. ~Kim
Contents |
Introduction
Lyme disease is caused by the spirochete Borrelia and spread via hard-bodied ticks belonging to the family Ixodidae. The Borrelia spirochetes are motile, helical organisms that contain outer surface proteins have several lipoproteins exposed on the surfaces of their membranes that invoke a response from host immune systems. The predominant group of these is classified as the outer surface proteins (Osps). Both the pathogenesis of Lyme disease as well as the host's immune response stem from the effects of the spirochete's presence and involvement in the system.[1]
The major strain of Borrelia in the United States is Borrelia burgdorferi sensu stricto (Bb.), with 20-100 cases of Lyme disease being reported per 100,000 people. In Europe, Lyme disease cases are more prevalent, with 100-130 diagnoses per 100,000 people, but instead are caused by the spirochetes Borrelia afzelii (Ba.) and Borrelia garinii (Bg.).[2]
The Ba. and & Bg. wiki pages are 'slightly sparse'; I don't know if we want to include those links or not... Also, do we want to mention the number of Borrelia strains but the fact that there are only 4 which are infectious to humans?
Lyme disease is a debilitating condition that begins with a characteristic bullseye rash known as an erythema migrans (EM) as well as the development of lesions on other parts of the body, not just at the site of the tick's attachment to its host. Secondary stage symptoms include affecting the heart, joints, and both the central and peripheral nervous systems. Borrelia have two major outer surface lipoproteins that are involved in Lyme disease: OspA and OspB. OspA is used in adhering to the tick's gut by binding with the tick receptor (TROSPA) Think a blurb about this would be useful- there isn't a wiki page for easy reference. During feeding, OspA is downregulated in order to evade an immune response from the incoming host blood into the gut, releasing the Borrelia from the gut wall and migrating into the tick's salivary glands, thereby allowing it to enter the host through the bite. This is evidenced by the fact that patients with Lyme disease have been found to not possess OspA antibodies in the early stages of the disease.[1][2] OspA is the protein most related to acute Lyme neuroborreliosis (LNB), the neurological manifestations of Lyme disease. We mention "two" proteins involved in Lyme Disease and just 'name' OspB but we don't even have a sentence or two about it in this part?
OspA & Lyme Disease
Acute Lyme Neuroborreliosis (LNB) is part of the second stage of Lyme disease in which the spirochete invades the peripheral and central nervous systems(CNS). Symptoms of LNB include: Bannwarth’s Syndrome, Lymphocytic Meningitis, and Cranial and Peripheral Neuritis. OspA is responsible for this complex inflammation process in the brain. Shouldn't we mention something about how OspA suppresses the immune system response and neutralize different effector mechanism systems?
When the Borrelia enter the CNS they encounter several different types of immune cells in the host body such as monocytes, macrophages, and dendritic cells. The immune cells then release proinflammatory cytokines as well as chemokines. There has been an observed increase in both these cytokines and chemokines in the CSF of patients suffering from LNB. Include some of the data that shows this? Also reference needed.
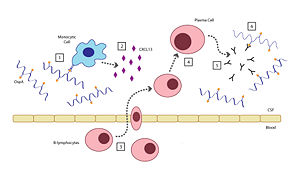
There are six steps involved in the host's inflammatory response to the presence of OspA: [2]
- Outer surface protein A (OspA) is recognized by a specific receptor on a monocytic cell.
- The OspA-bound monocytic cell releases the chemokine CXCL13.
- B-lymphocytes respond to the presence of the CXCL13 chemokines and move into the CSF.
- B-lymphocytes are turned into plasma cells. Add to this?
- The plasma cells create large amounts of anti-OspA antibodies and release them into the CSF.
- The anti-OspA antibodies bind to OspA on the spirochete, killing the Borrelia. This response can be helpful in killing Borrelia but also can
causeresult in harmful inflammation. Isn't it the presence of the chemokines that causes the development of LNB, not the antibodies?
OspA Vaccination
Lyme disease can be prevented avoided entirely by staying clear of areas with populations of ticks, wearing proper attire to minimize easily bitten areas, and using insect repellents containing DEET (N,N-diethy-m-toluamide). However, another effective means for prevention could be possible by using an outer surface protein from Borrelia in the development of a vaccine could also be an effective measure.[3]
Borrelia shows abundant abundance in OspA and OspB, and both of the proteins are very similar to each other; their amino acid sequences are 50% the same 1 . However OspA is more studied than OspB, and many studies related to OspA structure are developing and creating to make efficient vaccine against other Lyme diseases 4. The first vaccine against B. burgorferi sensu stricto was created targeting the OspA strain successfully 2 However this vaccine is unique in that it only works while Borrelia are still in the gut expressing OspA. (Ding) LYMErix, was discontinued in 2002 due to various weaknesses of the vaccine including its <80% efficacy, requirement for 3 doses, lack of data concerning the effects of the vaccine on children, and limitation of protection to the North American species of Borrelia. 6 To address this problem of international protection it would be helpful to create a chimera, mixing the OspA of different species. In order to do this the epitope of OspA should be studied. LA-2 <<SHOW FAB HIGHLIGHTED ON 1FJ1>> is a murine monoclonal antibody that binds strongly <<SHOW INTERACTION HIGHLIGHTED (ZOOMED IN) ON 1FJ1>> to OspA <<SHOW OSPA HIGHLIGHTED ON 1FJ1>>, and how effective a vaccine is correlated with LA-2 binding. 5
Structure of OspA
|
OspA is made of 21 anti-parallel β-strands and a single α-helix. 5 OspA is unique due to its dumbbell shape that contains two globular domains connected by a single layer β-sheet. 7 There are located at the C-terminus that are important in binding, and .
Loop 1 <<LOOP 1>>, residues 206 and 216, has an important role in binding due to a large exposed surface area, high mobility. Loop 2 <<LOOP 2>>, residues 224-233, and Loop 3 <<LOOP 3>>, residues 246-257, are also areas that are involved in binding. LA-2 recognizes OspA Bb, but does not recognize OspA from Bg.and Ba. Between Bb. and Ba. genetic sequences are generally invariant, but two residues change between the species, ALA 208 <<ALA 208>> in Bb. is GLN in Ba., and ASN 251 <<ASN 251>> in Bb. is ALA in Ba.. Bg. has more variation and in addition to the previous two differences, has at least one more difference, where ALA 215 <<ALA 215>> in Bb. is LYS, Bg. sometimes also has a deletion at Bb.’s ALA 208. LA-2 and OspA of Bb. form a tight interface when binding, and the longer GLN sidechain found in Ba. and Bg. is more difficult to accommodate, causing less binding. A chimera that was weakly recognized by LA-2 was made with parts of loop 1 from Bb., and loops 2 and 3 from Bg. 5 Recently, a different kind of chimera has been made which combined the proximal region of Bb. and distal region of Ba., and was able to successfully protect mice from both species. 8
Reference List of Available Scenes for OspA:
- (close up)
- (Ala208, Ala215 and Asn251 in B. burgdorferi, also hides R-groups)
- of Ala208, Ala215 and Asn251
In-Prog References
Not fully structured yet with -ref- tags, just organizing all reference information for ease
- 1 Connolly, SE and Benach JL. 2005. The Versatile Roles of Antibodies in Borrelia Infections. Microbiology 3: 411-420.
http://www.nature.com/nrmicro/journal/v3/n5/abs/nrmicro1149.html
PMID: 15864264 - 2 Rupprecht T, Koedel U, Fingerle V and Pfister H-W. 2008. The Pathogenesis of Lyme Neuroborreliosis: From Infection to Inflammation. Molecular Medicine 14(3-4): 205-212.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2148032/
PMID: 18097481 - 3 Nigrovic L, Thompson K. 2007. Epidemiology and Infection. The Lyme Vaccine: A Cautionary Tale. 135(1)1-8.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2870557/
PMID: 16893489 - 4 Battisti JM, Bono JL, Rosa PA, et al. 2008. Outer Surface Protein A Protects Lyme Disease Spirochetes from Acquired Host Immunity in the Tick Vector. Infect. Immun. 76(11): 5228-5237.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2573341/
PMID: 18779341 - 5 Ding W, Huang X, Yang X, Dunn J, et al. 2000. Structural Identification of a Key Protective B-Cell Epitope in Lyme Disease Antigen Osp A, Journal of Molecular Biology 302(5): 1153-1164.
http://www.sciencedirect.com/science/article/pii/S0022283600941196
PMID: 11183781 - 6 Plotkin S. 2011. Clinical Infectious Diseases. Correcting a Public Health Fiasco: The Need for a New Vaccine Against Lyme Disease. 52(3):s721-275.
- 7 Koide? Who used this?
- 8 Livey I, O’Rourke M, Traweger A, Savidis-Dacho H, Crowe B, Barrett P, Yang X, Dunn J, Luft B. 2011. Clinical Infectious Diseases. A new approach to a Lyme Disease Vaccine. 52(3):s266-s270.
References
- ↑ 1.0 1.1 Connolly SE, Benach JL. The versatile roles of antibodies in Borrelia infections. Nat Rev Microbiol. 2005 May;3(5):411-20. PMID:15864264 doi:10.1038/nrmicro1149
- ↑ 2.0 2.1 2.2 Rupprecht TA, Koedel U, Fingerle V, Pfister HW. The pathogenesis of lyme neuroborreliosis: from infection to inflammation. Mol Med. 2008 Mar-Apr;14(3-4):205-12. PMID:18097481 doi:10.2119/2007-00091.Rupprecht
- ↑ Nigrovic LE, Thompson KM. The Lyme vaccine: a cautionary tale. Epidemiol Infect. 2007 Jan;135(1):1-8. Epub 2006 Aug 8. PMID:16893489 doi:10.1017/S0950268806007096
External Links
- World Health Organization: Lyme Disease
- PubMed Health: Lyme Disease
- American Lyme Disease Foundation