User:Marvin O'Neal/OspA
From Proteopedia
| Line 57: | Line 57: | ||
</p> | </p> | ||
| - | <Structure load="1fj1" size="350" frame="true" align="right" name="complex" caption="Outer surface protein A (OspA) in complex with the LA-2 Fab antibody ([[1fj1|1FJ1]])."> | + | <Structure load="1fj1" size="350" frame="true" align="right" name="complex" caption="Outer surface protein A (OspA) in complex with the LA-2 Fab antibody ([[1fj1|1FJ1]])." scene="Studio:G2SecL03/Ospafab-orig/1"> |
<p> | <p> | ||
Revision as of 17:03, 2 May 2012
|
Outer Surface Protein A (OspA) is a major lipoprotein found on the surface of spirochetes from the genus Borrelia and is comprised of 21 anti-parallel β-sheets and a single α-helix. OspA's expression is regulated at different points in time, from being downregulated during the tick's feeding process on its host to being upregulated in the host's cerebrospinal fluid (CSF) to induce inflammatory response, resulting in acute Lyme neuroborreliosis. OspA has also been used as a vector in working towards the development of a vaccine for Lyme disease.
Introduction
Lyme disease is caused by the spirochete Borrelia and spread via hard-bodied ticks belonging to the family Ixodidae. The Borrelia spirochetes are motile, helical organisms have several lipoproteins exposed on the surfaces of their membranes that invoke a response from host immune systems. The predominant group of these is classified as the outer surface proteins (Osps). Both the pathogenesis of Lyme disease as well as the host's immune response stem from the effects of the spirochete's presence and involvement in the system.[1] The major strain of Borrelia in the United States is Borrelia burgdorferi sensu stricto (Bb.), with 20-100 cases of Lyme disease being reported per 100,000 people. In Europe, Lyme disease cases are more prevalent, with 100-130 diagnoses per 100,000 people, but are caused by the spirochetes Borrelia afzelii (Ba.) and Borrelia garinii (Bg.) in addition to B. burgdorferi.[2][3]
Lyme disease is a debilitating condition that begins with a characteristic bullseye rash known as an erythema migrans (EM) as well as the development of lesions on other parts of the body, not just at the site of the tick's attachment to its host. Secondary stage symptoms include affecting the heart, joints, and both the central and peripheral nervous systems. Borrelia has two major outer surface lipoproteins that are involved in Lyme disease: OspA and OspB. OspA is used in adhering to the tick's gut by binding with the tick receptor (TROSPA) During feeding, OspA is downregulated in order to evade an immune response from the incoming host blood into the gut, releasing the Borrelia from the gut wall and migrating into the tick's salivary glands, thereby allowing it to enter the host through the bite. This is evidenced by the fact that patients with Lyme disease have been found to not possess OspA antibodies in the early stages of the disease.[1][2] OspA is the protein most related to acute Lyme neuroborreliosis (LNB), the neurological manifestations of Lyme disease.
Once inside the host, the Borrelia has a great number of mechanisms available to actively suppress the host's immune system response and neutralize its effector mechanisms, such as the expression of another outer surface protein, OspC, which prevents susceptibility to the host's innate immunity and complement systems. Additionally, Borrelia is capable of suppressing many of its surface proteins to reduce its detectability, but can also utilize protective means by temporarily expressing them when needed.
OspA & Lyme Disease
Acute Lyme Neuroborreliosis (LNB) is part of the second stage of Lyme disease in which the spirochete invades the peripheral and central nervous systems (CNS). Symptoms of LNB include: Bannwarth’s Syndrome, Lymphocytic Meningitis, and Cranial and Peripheral Neuritis. The presence of OspA in the cerebrospinal fluid (CSF) is responsible for this complex inflammatory response in the brain that leads to the neuroborreliosis.
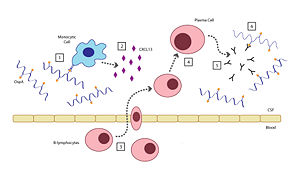
There are six steps involved in the host's inflammatory response to OspA: [2]
- When the Borrelia enter the host’s CNS they encounter several different types of immune cells such as monocytes, macrophages, and dendritic cells. While in the CSF, outer surface protein A (OspA) is upregulated and it’s increased expression promotes recognition by a specific receptor on a monocyte.
- The OspA-bound monocyte then releases proinflammatory cytokines (i.e. interferon), as well as chemokines, such as CXCL13. In patients with LNB, there is an observed increase in the levels of these cytokines and chemokines in their CSF. The production of chemokines leads to the recruitment of other immune cells to the site of infection.
- B-lymphocytes respond to the new concentration gradient of CXCL13 between the blood and CSF and migrate into the CSF.
- B-lymphocytes undergo receptor-mediated endocytosis, consuming the OspA antigens present in the CSF, thereby triggering its activation. The B-lymphocytes then are able to differentiate and mature into plasma cells.
- The plasma cells create large quantities of anti-OspA antibodies specific to this strain of Borrelia and release them into the CSF.
- The anti-OspA antibodies will then bind to the OspA on the spirochete’s membrane, thus killing the Borrelia.
This process is two-sided in the sense that the OspA aids in the pathogenesis of new symptoms (neuroborreliosis) through the chemokine’s actions, as well as initiating the signaling cascade to destroy itself.
OspA Vaccination
Risk of developing Lyme disease can be mitigated by staying clear of areas with populations of ticks, wearing proper attire to minimize easily bitten areas of the body, and using insect repellents containing DEET (N,N-diethy-m-toluamide). However, another effective means for prevention could be possible by using an outer surface protein from Borrelia in the creation of a vaccine.[4]
The membrane composition of Borrelia is abundant in both OspA and OspB, and the two proteins share a 53% similarity in their primary sequences. Both OspA and OspB are expressed in the tick's gut and downregulated during feeding and aid in its survivability; however, OspA is overall less varied and reactive than OspB, which has greater variability.[5] The relatively conserved sequence of OspA thus lends itself better to study and application toward the development of a vaccine for a broader range of Borrelia strains in the treatment of Lyme disease than that of OspB. The first vaccine used a purified recombinant form of OspA and functioned in blocking transmission of the spirochetes expressing OspA from tick to host during feeding, killing them while still attached to the tick's gut.[1][6] The vaccine, Lymerix, had shown 76% and 92% effectiveness in separate clinical trials in which patients were treated for two years following a three-dose schedule. However, the vaccination was suspended from use in 2002 when opponents claimed the IgG antibodies for OspA were associated with the onset of severe chronic arthritis, as well as other side effects affecting immunity.[1][7] This fact, in conjunction with the desire for a more widespread vaccine treating multiple strains of Borrelia, has spurred research towards a new vaccine.
| |||||||||||