Herceptin - Mechanism of Action
From Proteopedia
| Line 40: | Line 40: | ||
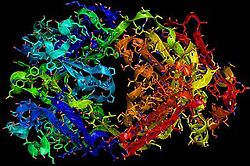
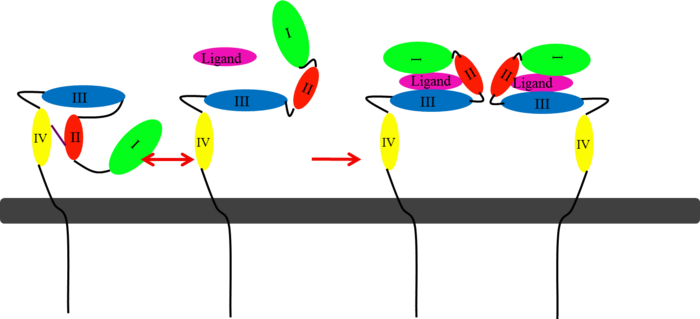
HER2 structure differs in that subdomains I and III are in constant contact resulting in a permanent open conformation <ref name="two"/><ref name="three"/>. Subdomains I and III in HER2 are stabilized by core hydrophobic residues surrounded by hydrophilic contacts facilitating the stabilization of this interaction <ref name="two"/>. This fixed conformation allows the receptor to act in a ligand-independent manner and permits the access of subdomain II for dimerization. Perhaps this may explain why a high-affinity ligand for HER2 has not yet been recognized. The absence of subdomain II and IV contact can be explained by the mutations of Gly 563 and His 565 found in the other members of the HER family to Pro and Phe respectively. Since subdomain II is always available for dimerization it is free to form heterodimers with any of the other epidermal growth factor receptors. Asp 285 is the only residue in subdomain II not conserved between EGFR and HER2. Leu replaces Asp 285 in HER2 and can explain why HER2 forms homodimers to a lesser extent. Once dimerized, HER2 activates the MAPK pathway, which in turn initiates cell proliferation, migration, differentiation, and angiogenesis <ref name="three"/>. | HER2 structure differs in that subdomains I and III are in constant contact resulting in a permanent open conformation <ref name="two"/><ref name="three"/>. Subdomains I and III in HER2 are stabilized by core hydrophobic residues surrounded by hydrophilic contacts facilitating the stabilization of this interaction <ref name="two"/>. This fixed conformation allows the receptor to act in a ligand-independent manner and permits the access of subdomain II for dimerization. Perhaps this may explain why a high-affinity ligand for HER2 has not yet been recognized. The absence of subdomain II and IV contact can be explained by the mutations of Gly 563 and His 565 found in the other members of the HER family to Pro and Phe respectively. Since subdomain II is always available for dimerization it is free to form heterodimers with any of the other epidermal growth factor receptors. Asp 285 is the only residue in subdomain II not conserved between EGFR and HER2. Leu replaces Asp 285 in HER2 and can explain why HER2 forms homodimers to a lesser extent. Once dimerized, HER2 activates the MAPK pathway, which in turn initiates cell proliferation, migration, differentiation, and angiogenesis <ref name="three"/>. | ||
| - | A particularly harmful form of HER2 can exist within the cell membrane | + | A particularly harmful form of HER2 can exist within the cell membrane along with the other HER members<ref name="twelve">Gajria, Devika, and Sarat Chandarlapaty. HER2-amplified Breast Cancer: Mechanisms of Trastuzumab 11.2 (2011): 263-75. National Institute of Health. Web. Oct. 2012. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3092522/pdf/nihms289124.pdf>.</ref>. The juxtamembrane region of the extracellular domain is prone to proteolytic cleavage resulting in a protein called p95HER2. <scene name='Sandbox_reserved_Herceptin/Truncated/1'>p95HER2</scene> is the truncated form of HER2 and has been shown to have an increased ability to cross-phosphorylate with the other receptors of the HER family and has increased cellular signaling capabilities. |
One combination of epidermal growth factor receptors has the potential to be a potent inducer of tumorigenesis <ref name="three"/>. HER2:HER3 combination can be especially detrimental to a patient exhibiting over-expression of HER2. While HER2 activates a cell proliferation pathway, HER3 is the only receptor that can directly activate the PI3K pathway. The PI3K pathway recruits its messengers (Akt and mTOR) that allows for the activation of cell survival mechanisms and helps the cell resist apoptosis. This combination can become deadly resulting in metastasized cancer. | One combination of epidermal growth factor receptors has the potential to be a potent inducer of tumorigenesis <ref name="three"/>. HER2:HER3 combination can be especially detrimental to a patient exhibiting over-expression of HER2. While HER2 activates a cell proliferation pathway, HER3 is the only receptor that can directly activate the PI3K pathway. The PI3K pathway recruits its messengers (Akt and mTOR) that allows for the activation of cell survival mechanisms and helps the cell resist apoptosis. This combination can become deadly resulting in metastasized cancer. | ||
| Line 54: | Line 54: | ||
*inhibition of angiogenesis | *inhibition of angiogenesis | ||
| - | When Herceptin binds to HER2 it is able to flag these cells for destruction. This works by | + | When Herceptin binds to HER2 it is able to flag these cells for destruction<ref name="two"/><ref name="three"/><ref name="twelve"/>. This works by |
attracting lymphocytes to these HER2+ cells. Lymphocytes are then stimulated to release substances that cause cellular apoptosis. | attracting lymphocytes to these HER2+ cells. Lymphocytes are then stimulated to release substances that cause cellular apoptosis. | ||
| - | An added significant mechanism of action of Herceptin is the prevention of the formation of p95HER2. By binding to the juxtamembrane region Herceptin sterically hinders any cleavage of the site ultimately preventing the formation of the highly active p95HER2. | + | An added significant mechanism of action of Herceptin is the prevention of the formation of p95HER2<ref name="two"/><ref name="three"/><ref name="twelve"/>. By binding to the juxtamembrane region Herceptin sterically hinders any cleavage of the site ultimately preventing the formation of the highly active p95HER2. |
| - | The next two mechanisms of action for Herceptin involve intracellular inhibition. By the binding of Herceptin to the extracellular region of HER2 Herceptin is able to prevent downstream activation of cell signals that induce cell proliferation and angiogenesis. By repression of the proangiogenic factors Herceptin is also able to induce antiangiogenic factors. Inhibiting these intracellular processes Herceptin prevents any further blood vessels from developing towards the tumor and prevents the tumor from growing any larger. | + | The next two mechanisms of action for Herceptin involve intracellular inhibition<ref name="two"/><ref name="three"/><ref name="twelve"/>. By the binding of Herceptin to the extracellular region of HER2 Herceptin is able to prevent downstream activation of cell signals that induce cell proliferation and angiogenesis. By repression of the proangiogenic factors Herceptin is also able to induce antiangiogenic factors. Inhibiting these intracellular processes Herceptin prevents any further blood vessels from developing towards the tumor and prevents the tumor from growing any larger. |
One limitation with this therapy is that it does not prevent HER2 from dimerizing with HER3 <ref name="three"/>. This makes it possible for the activation of the PI3K pathway which increases the ability of the cell to survive. Further therapies targeting the prevention of HER2 to dimerize with other members of the HER family will be necessary for future investigational studies. | One limitation with this therapy is that it does not prevent HER2 from dimerizing with HER3 <ref name="three"/>. This makes it possible for the activation of the PI3K pathway which increases the ability of the cell to survive. Further therapies targeting the prevention of HER2 to dimerize with other members of the HER family will be necessary for future investigational studies. | ||
Revision as of 17:31, 15 November 2012

Basics
Introduction
Breast cancer is the most common type of cancer found among women except for skin cancers[1]. Although it is rarely seen in men, one in eight women will be diagnosed with breast cancer within their lifetime. Patients exhibiting an over-expression in Human Epidermal Growth Factor Receptor 2 (HER2) account for 25% of all breast cancer [2][3]. HER2+ patients often experience a more aggressive cancer resulting in more metastasized tumors [3]. The statistics show a poor prognosis for HER2+ patients with a 5-year survival rate of 68%. Herceptin (also known as trastuzumab) was approved by the FDA in September of 1998 for HER2+ patients and has been shown to be an effective tool in the battle against breast cancer [4].
HER2
HER2 is one of four human epidermal growth factor receptors (EGFR , HER2, HER3, and HER4)[5][6]. These receptors are part of a family of receptor tyrosine kinases responsible for cell proliferation and differentiation[2][7].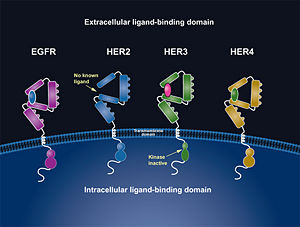
These human epidermal growth factor receptors exist on the cell surface and, with the exception of HER2, bind to specific ligands (epidermal growth factors) [2]. Over 11 different ligands for the epidermal growth factor receptors have been identified [5]. After binding with these ligands the HER family is able to homodimerize or heterodimerize with one another [8]. Dimerization is a chemical interaction between two "like" molecules in which they form a union. This dimerization causes a cross-phosphorylation of the intracellular tyrosine kinases between the two receptors and ultimately activates a cell signaling pathway.
HER2 is the only receptor within this family that is constitutively active being able to dimerize with other HER family members acting in a ligand-independent manner [2][8]. This continuous activation of the cell signal pathway causes an increase in cell division; thus, potentially causing a tumor. [8]
Herceptin
Herceptin, generic trastuzumab, is a monoclonal antibody (refer to figure 3)[10]. Herceptin is an effective treatment for breast cancer for the reason that it binds to the extracellular domain of HER2 and by multiple mechanisms of action can prevent cell proliferation as well as target these HER2+ cells for destruction by the immune system [3][10].
| |||||||||||
References
- ↑ "What Are the Key Statistics about Breast Cancer?" Breast Cancer. Cancer.org, 31 Oct. 2012. Web. Nov. 2012. <http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-key-statistics>.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 Cho, Hyun-Soo, Karen Mason, Kasra X. Ramyar, Ann Marie Stanley, Sandra B. Gabelli, Dan W. Denney, Jr., and Daniel J. Leahy. "Structure of the Extracellular Region of HER2 Alone and in Complex with the Herceptin Fab." Letters to Nature 421 (2003): 756-60. PubMed.gov. Web. Oct. 2012.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 "HER2 Dimerization: A Key Component of Oncogenic Signaling in HER2 Breast Cancer." HER2+ Breast Cancer. Genentech, n.d. Web. 09 Nov. 2012. <http://www.biooncology.com/research-education/hdis/her2-dimerization/index.html>.
- ↑ "Herceptin Development Timeline." Genentech: Medicines. Genentech, n.d. Web. Nov. 2012. <http://www.gene.com/gene/products/information/oncology/herceptin/timeline.html>.
- ↑ 5.0 5.1 Bazley, L. A., and W. J. Gullick. "The Epidermal Growth Factor Receptor Family." Endocrine-Related Cancer. Society for Endocrinology and European Society of Endocrinology, 2005. Web. Oct. 2012. <http://erc.endocrinology-journals.org/content/12/Supplement_1/S17.full>.
- ↑ 6.0 6.1 Satyanarayanajois, Seetharama, Stephanie Villalba, Liu Jianchao, and Go Mei Lin. "Design, Synthesis, and Docking Studies of Peptidomimetics." Chem. Biol. Drug Des. 74.3 (2009): 246-57. National Institute of Health. Web. Nov. 2012. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2866155/pdf/nihms-190276.pdf>.
- ↑ Banappagari, Sashikanth, Sharon Ronald, and Seetharama Satyanarayanajois. "Structure-activity Relationship of Conformationally Constrained." Medchemcomm. 2.8 (2011): 752-59. National Institute of Health. Web. Oct. 2012. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3163471/pdf/nihms308284.pdf>.
- ↑ 8.0 8.1 8.2 8.3 "HER Pathways Are of Critical Importance in Cancer." HER Receptors Overview. Genentech, n.d. Web. 09 Nov. 2012. <http://www.biooncology.com/research-education/her/overview/index.html>.
- ↑ Ryzhkov, Andrew. "Trastuzumab." Wikipedia. Wikimedia Foundation, 11 Aug. 2012. Web. 09 Nov. 2012. <http://en.wikipedia.org/wiki/Trastuzumab>.
- ↑ 10.0 10.1 Jiang, Beihai, Wenbin Liu, Hong Qu, Lin Meng, Shumei Song, Tao Ouyang, and Chengchao Shou. "A Novel Peptide Isolated from a Phage Display Peptide Library with." The Journal of Biological Chemistry 280.6 (2005): 4656-662. The Journal of Biological Chemistry. Web. Oct. 2012. <http://www.jbc.org/content/280/6/4656.full.pdf+html>.
- ↑ 11.0 11.1 "ERBB2." Genetics Home Reference. U.S. National Library of Medicine, 5 Nov. 2012. Web. 09 Nov. 2012. <http://ghr.nlm.nih.gov/gene/ERBB2>.
- ↑ 12.0 12.1 12.2 Lammerts Van Bueren, Jeroen, Wim K. Bleeker, Annika Bra¨ Nnstro¨m, Anne Von Euler, Magnus Jansson, Matthias Peipp, Tanja Schneider-Merck, Thomas Valerius, Jan G. J. Van De Winkel, and Paul W. Parren. "The Antibody Zalutumumab Inhibits Epidermal Growth." PNAS 105.16 (2008): 6109-114. Web. Nov. 2012. <http://www.pnas.org/content/105/16/6109/F1.expansion.html>.
- ↑ Saxon, Marian L., and David C. Lee. "Mutagenesis Reveals a Role for Epidermal Growth Factor Receptor Extracellular Subdomain IV in Ligand Binding." The Journal of Biological Chemistry 274.40 (1999): 28356-8362. PubMed.gov. Web. Oct. 2012. <http://www.jbc.org/content/274/40/28356.long>.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 Gajria, Devika, and Sarat Chandarlapaty. HER2-amplified Breast Cancer: Mechanisms of Trastuzumab 11.2 (2011): 263-75. National Institute of Health. Web. Oct. 2012. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3092522/pdf/nihms289124.pdf>.