Sandbox WWC3
From Proteopedia
| Line 3: | Line 3: | ||
<Structure load='5EK0' size='350' frame='true' align='right' caption='Insert caption here' scene='Insert optional scene name here' /> | <Structure load='5EK0' size='350' frame='true' align='right' caption='Insert caption here' scene='Insert optional scene name here' /> | ||
==Function== | ==Function== | ||
| - | Sodium channels initiate action potentials in nerve and muscle cells. These electrical signals initiate the contraction of muscles and the release of neurotransmitters. The electrical signal is propagated when the sodium channel allows the influx of sodium ions. These positively charged ions depolarize the resting membrane potential of -70mV to +40mV, which creates the electrical signal that is sent along the length of the cell.The initial influx of sodium ions is often activated by the binding of a neurotransmitter to receptors on the post-synaptic membrane. <ref>https://en.wikipedia.org/wiki/Neurotransmission</ref> Then, as the sodium ions depolarize the membrane potential. more sodium channels open, and the action potential moves along the length of the muscle or nerve. The channels inactivate after 1-2ms and the depolarization is then reversed by the efflux of potassium ions out of potassium channel. <ref name ="sod"/> This information was first discovered by Hodgkin and Huxley in 1952. <ref name ="physio">https://en.wikipedia.org/wiki/Hodgkin%E2%80%93Huxley_model> For more information on the role of sodium channels in electrical signaling, click [https://en.wikipedia.org/wiki/Action_potential here]. | + | Sodium channels initiate action potentials in nerve and muscle cells. These electrical signals initiate the contraction of muscles and the release of neurotransmitters. The electrical signal is propagated when the sodium channel allows the influx of sodium ions. These positively charged ions depolarize the resting membrane potential of -70mV to +40mV, which creates the electrical signal that is sent along the length of the cell.The initial influx of sodium ions is often activated by the binding of a neurotransmitter to receptors on the post-synaptic membrane. <ref>https://en.wikipedia.org/wiki/Neurotransmission</ref> Then, as the sodium ions depolarize the membrane potential. more sodium channels open, and the action potential moves along the length of the muscle or nerve. The channels inactivate after 1-2ms and the depolarization is then reversed by the efflux of potassium ions out of potassium channel. <ref name ="sod"/> This information was first discovered by Hodgkin and Huxley in 1952. <ref name ="physio">https://en.wikipedia.org/wiki/Hodgkin%E2%80%93Huxley_model</ref> For more information on the role of sodium channels in electrical signaling, click [https://en.wikipedia.org/wiki/Action_potential here]. |
==Structure== | ==Structure== | ||
Current revision
Sodium channels are voltage gated integral membrane proteins found in muscles and neurons that selectively allow for the diffusion of sodium ions across the membrane. [1]These proteins are important for all cells but are specifically responsible for initiating electrical signaling in these cells, which causes action potentials or muscle contractions.[2] Sodium channels and are commonly targets of drugs and mutations can cause serious disease. Each sodium channel is composed of three subunits: the alpha subunit, which is the transmembrane ion channel, and two beta subunits that modulate channel gating and regulate the channel expression in the membrane. [3] [1] The alpha subunit is able to function independently of the beta subunit. [3]
|
Contents |
Function
Sodium channels initiate action potentials in nerve and muscle cells. These electrical signals initiate the contraction of muscles and the release of neurotransmitters. The electrical signal is propagated when the sodium channel allows the influx of sodium ions. These positively charged ions depolarize the resting membrane potential of -70mV to +40mV, which creates the electrical signal that is sent along the length of the cell.The initial influx of sodium ions is often activated by the binding of a neurotransmitter to receptors on the post-synaptic membrane. [4] Then, as the sodium ions depolarize the membrane potential. more sodium channels open, and the action potential moves along the length of the muscle or nerve. The channels inactivate after 1-2ms and the depolarization is then reversed by the efflux of potassium ions out of potassium channel. [1] This information was first discovered by Hodgkin and Huxley in 1952. [5] For more information on the role of sodium channels in electrical signaling, click here.
Structure
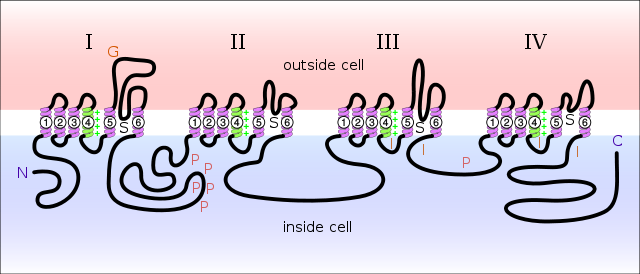
As noted above, the sodium channel consists of an alpha and two beta subunits. However, the alpha subunit is the only part necessary for the function of the channel. [1] The alpha subunit, depicted right, consists of four repeating structures, named I through IV and shown in different colors . [6] These structures consist of six transmembrane alpha helices named S1 through S6. [6] Interestingly, each repeating subunit resembles a bacterial K+ channel. [6] These subunits fold together to form a central pore, and this complete structure resembles a bacterial Ca2+ channel. [6]
Gating
The S1 through S4 segments make up the gating mechanism. [2] In particular, the S4 segments consist of repeated motifs of a positively charged residue (usually Arg) followed by two hydrophobic residues. [2] This alpha helix is exposed to the membrane electric field, and in response to a depolarization, it is displaced outwards, causing the channel to open.[2] S4 segments can be seen in red . Surprisingly, each S4 chain does not contribute equally to the gating of this channel. A mutation in one chain may have a much larger effect than a mutation in another S4 chain. [2] However, these S4 segments are merely sensors. The actual gating mechanism is still up for debate, with the leading contender being the S6 segment. This mechanism would be similar to the gating of the K+ channel. [6] The outward movement of the S4 segment moves the S4-S5 linker, which pulls the S5-S6 segments and opens the pore. [2] Overall, the voltage sensing domain makes a rolling motion of the S4-S5 linker around the pore. [2] The S4-S5 linker can be seen .
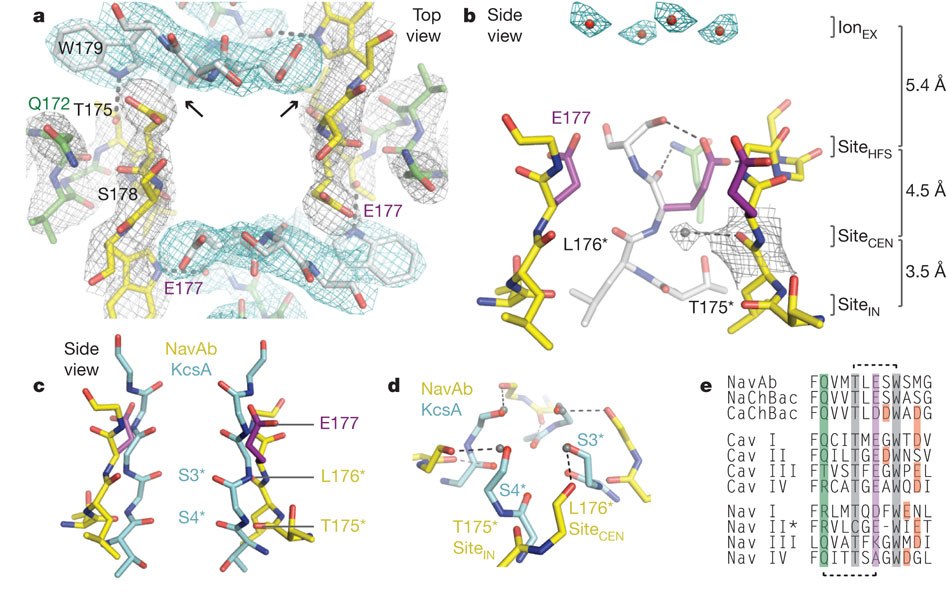
Selectivity Filter
This channel conducts sodium at nearly the rate of free diffusion. [2] This pore consists of an outer funnel-like vestibule, a selectivity filter, a central cavity, and an intracellular activation gate. [2] Unlike the K+ channel, the Na+ channel conducts sodium ions that are hydrated with four water molecules. [2] Much like with the gating mechanism, each domain does not contribute equally to the selectivity of the pore, but the channel selects for sodium 100x greater than it selects for any other ion. [6] It is likely that the sodium ion can get much closer to the channel entry than a larger K+ ion. When the ion reaches this distance, there is a more efficient removal of water and the sodium interacts with the Glu117 side chains. Two side chains interact directly with the sodium ion and two additional side chains form hydrogen bonds with the water molecules [2]. The pore is made up of T175, L176, E177 and S178. [2] The Glu side chains act as hydrogen bond acceptors two in-plane molecules surrounding the sodium ion. [2] The other two water molecules would be axial to the sodium ion. [2] Full rehydration would occur when the ion moves next to the Leu and Thr residues. [2] Full rehydration then allows the sodium ion to enter the cytoplasm. [2]
To see the selectivity filter, click . T175 is blue, L176 is yellow, E177 is red and S178 is black.
This image shows the crystal structure of the selectivity filter. [2]
α Subunits
There are nine different α subunits named NaV1.1 through NAV1.9. [1] Genes are SCN1 through SCN11. [1] These structures differ in their sequence and kinetics. [1] As stated above, the α subunit is necessary to the function of the channel and can function independently of the β subunit. You can find the structures and more information below.
- NaV1.1: found in central and peripheral neurons and myocytes. Click for the structure of the NaV1.1 inactivation gate. [1]
- NaV1.2: found in central and peripheral neurons. Click for the structure of the NaV1.2 C terminal domain in complex with FGF13U and Ca2+/calmodulin. [1]
- NaV1.3: found in central and peripheral neurons and cardiac myocytes. [1]
- NaV1.4: found in skeletal muscle. [1]
- NaV1.5: found in cardiac myocytes, uninnervated skeletal muscle, central neurons, gastrointestinal smooth muscle cells, and interstitial cells of Cajal. Click for the structure of the NaV1.5 C terminal domain in complex with FGF12B and Ca2+/calmodulin. [1]
- NaV1.6: found in central neurons, dorsal root ganglia, peripheral neurons, heart and glial cells. [1]
- NaV1.7: found in dorsal root ganglia, sympathetic neurons, Schwann cells and neuroendocrine cells. [1]
- NaV1.8: found in dorsal root ganglia. [1]
- NaV1.9: found in dorsal root ganglia. [1]
β Subunits
Beta subunits function in channel gating, channel expression and form links to the cytoskeleton. [1] There are four different beta subunits named NaVβ1 through NaVβ4 and the genes are named SCN1B through SCN4B. [1]
- NaVβ1: Assembles with NaV1.1 and NaV1.7 and found in central and peripheral neurons, skeletal muscle, heart and glial cells. [1]
- NaVβ2: Assembles with NaV1.1, NaV1.2, NaV1.5 and NaV1.7 and found in central and peripheral neurons, heart and glial cells. [1]
- NaVβ3: Assembles with NaV1.1, NaV1.3 and NaV1.5 and found in the central and peripheral neurons, adrenal gland and heart. [1]
- NaVβ4: Assembles with NaV1.1, NaV1.2, and NaV1.5 and found in the heart, skeletal muscles, central and peripheral neurons. [1]
Medical Implications
Diseases caused by mutations in sodium channels can come in many forms. Some mutations affect skeletal, cardiac or smooth muscle, while others affect neural function. Common diseases include long QT syndrome, hyperkalemic periodic paralysis, hypokalemic periodic paralysis, myotonia fluctuans and myotonia permanens among many others. [7]
Long QT Syndrome
This disease causes seizures, fainting or sudden death from cardiac arrhythmias and is caused my a mutation in the SCN5A gene, or the gene that encodes the NaV1.5 alpha subunit. [8][9] It was found that this deletion includes residues 1505-1507 (KPQ).[8] These residues occur in the cytoplasmic linker between domain III and domain IV. [8]
Hyperkalemic Periodic Paralysis
Hyperkalemic period paralysis is caused by the mutations T704M, S906T, A1156T, M1360V, A1448C and/or M1592V. [10] These mutations cause periodic or permanent weakness. [10] Physiologically, this is a gain of function mutation. During rest after exercise, or after eating foods rich in K+, the extracellular K+ increases, which mildly depolarizes the membrane.[10] This causes abnormal Na+ channels to open, and they are unable to inactivate. [10] This sustained depolarization of the membrane causes even more abnormal Na+ channels to open and ultimately this leads to loss of excitability and weakness. [10] This symptom usually appears within the first decade of life and can be aggravated by exercise, cold, potassium loading, fasting or pregnancy. [10] Attacks are usually brief and do not need treatment. [10]
Hypokalemic Periodic Paralysis
Hypokalemic periodic paralysis is caused by the mutations R669H, R672H, R672G, R672S, R1132Q, and/or P1158S in the S4 segment of the NaV1.4 sodium channel. [11] This disease is caused by a loss of function mutation resulting in attacks of muscular weakness. [11] This disorder is a dominant mutation. [12] Factors that trigger these episodes include meals rich in carbohydrates, rest after exercise, early morning hours, and emotional stress. [12] Most mutations are in two the Arg residues closes to the extracellular side of the S4 segment. [12] These mutations cause a leak current of Na+ ions inward, which is called an "omega" current. [12] This inward current causes the K+ channels to not be effective and results in muscle weakness. [12]
Myotonia Fluctuans
Myotonia fluctuans is due to the G1306A mutation in the NaV1.4 sodium channel. [13] All mutations at the 1306 site cause reduced channel inactivation due to the fact that the residue is located on the hinge of the channel inactivation gate. [13] This disease is characterized by the inability to relax voluntary muscle after vigorous exercise. However, the condition fluctuates day to day, hence the name. [13]
Myotonia Permanens
Myotonia permanens is similar to myotonia fluctuans in that it causes the inability to relax voluntary muscle. [13] However, this disease is caused by the G1306Q mutation. [13] Again, this mutation causes reduced channel inactivation due to the location of the mutation on the inactivation gate. [13] Severe myotonia permanens may interfere with respiration and is worsened after eating K+ rich foods. [13]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 https://en.wikipedia.org/wiki/Sodium_channel
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 Payandeh J, Scheuer T, Zheng N, Catterall WA. The crystal structure of a voltage-gated sodium channel. Nature. 2011 Jul 10;475(7356):353-8. doi: 10.1038/nature10238. PMID:21743477 doi:10.1038/nature10238
- ↑ 3.0 3.1 Isom LL. Sodium channel beta subunits: anything but auxiliary. Neuroscientist. 2001 Feb;7(1):42-54. PMID:11486343
- ↑ https://en.wikipedia.org/wiki/Neurotransmission
- ↑ https://en.wikipedia.org/wiki/Hodgkin%E2%80%93Huxley_model
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Marban E, Yamagishi T, Tomaselli GF. Structure and function of voltage-gated sodium channels. J Physiol. 1998 May 1;508 ( Pt 3):647-57. doi: 10.1111/j.1469-7793.1998.647bp.x. PMID:9518722 doi:http://dx.doi.org/10.1111/j.1469-7793.1998.647bp.x
- ↑ http://neuromuscular.wustl.edu/mother/chan.html#SCN4A
- ↑ 8.0 8.1 8.2 doi: https://dx.doi.org/10.1016/0092-8674(95)90359-3
- ↑ http://www.mayoclinic.org/diseases-conditions/long-qt-syndrome/basics/definition/con-20025388
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 http://neuromuscular.wustl.edu/mother/activity.html#hrpp
- ↑ 11.0 11.1 http://neuromuscular.wustl.edu/mtime/mepisodic.html#hopp
- ↑ 12.0 12.1 12.2 12.3 12.4 Groome JR, Lehmann-Horn F, Fan C, Wolf M, Winston V, Merlini L, Jurkat-Rott K. NaV1.4 mutations cause hypokalaemic periodic paralysis by disrupting IIIS4 movement during recovery. Brain. 2014 Apr;137(Pt 4):998-1008. doi: 10.1093/brain/awu015. Epub 2014 Feb 18. PMID:24549961 doi:http://dx.doi.org/10.1093/brain/awu015
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 http://neuromuscular.wustl.edu/mother/activity.html#mf