We apologize for Proteopedia being slow to respond. For the past two years, a new implementation of Proteopedia has been being built. Soon, it will replace this 18-year old system. All existing content will be moved to the new system at a date that will be announced here.
Sandbox Reserved 1774
From Proteopedia
(Difference between revisions)
| Line 7: | Line 7: | ||
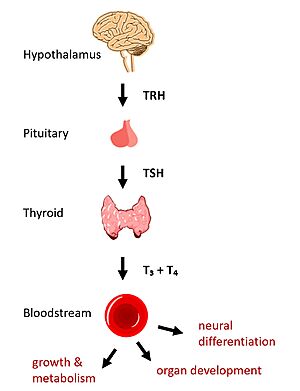
[[Image:HPT Axis.jpg|300 px|right|thumb|Figure 1: TSHR binds TSH in the HPT signaling axis pathway, which regulates metabolism and growth.]] | [[Image:HPT Axis.jpg|300 px|right|thumb|Figure 1: TSHR binds TSH in the HPT signaling axis pathway, which regulates metabolism and growth.]] | ||
In humans, the hypothalamic-pituitary-thyroid (HPT) signaling axis regulates functions including metabolism, growth, organ development, and neural differentiation <ref name="Brent">Brent GA. Mechanisms of thyroid hormone action. J Clin Invest. 2012;122(9):3035-3043. [https://doi.org/10.1172/JCI60047 DOI: 10.1172/JCI60047]</ref>. In this pathway, the thyroid stimulating hormone receptor (TSHR) activates transcription of thyroid hormones in response to ligand binding by thyroid stimulating hormone (TSH). After a brief introduction to the biological significance of TSHR, this page explores the structure of TSHR and its significance to TSH binding and receptor activation. | In humans, the hypothalamic-pituitary-thyroid (HPT) signaling axis regulates functions including metabolism, growth, organ development, and neural differentiation <ref name="Brent">Brent GA. Mechanisms of thyroid hormone action. J Clin Invest. 2012;122(9):3035-3043. [https://doi.org/10.1172/JCI60047 DOI: 10.1172/JCI60047]</ref>. In this pathway, the thyroid stimulating hormone receptor (TSHR) activates transcription of thyroid hormones in response to ligand binding by thyroid stimulating hormone (TSH). After a brief introduction to the biological significance of TSHR, this page explores the structure of TSHR and its significance to TSH binding and receptor activation. | ||
| - | + | ||
== Biological Significance of TSHR == | == Biological Significance of TSHR == | ||
The HPT signaling axis involves the brain, thyroid gland, and bloodstream circulation. In the first step of the pathway, thyrotropin releasing hormone (TRH) is secreted by the hypothalamus, which in turn stimulates the anterior pituitary gland to produce TSH <ref name="Brent" />. TSH binds to TSHR on the surface of thyroid cells and triggers the production of thyroid hormones thyroxine (T3) and triiodothyronine (T4) through G-protein coupled receptor (GPCR) signaling <ref name="Chu">Chu YD, Yeh CT. The Molecular Function and Clinical Role of Thyroid Stimulating Hormone Receptor in Cancer Cells. Cells. 2020;9(7):1730. [https://doi.org/10.3390/cells9071730 DOI:10.3390/cells9071730]</ref>. T3 and T4 circulate in the bloodstream and enter cells via thyroid hormone transporters to regulate metabolic functions. Additionally, T3 and T4 act in a negative feedback loop to inhibit further TSH production <ref name="Brent" />. | The HPT signaling axis involves the brain, thyroid gland, and bloodstream circulation. In the first step of the pathway, thyrotropin releasing hormone (TRH) is secreted by the hypothalamus, which in turn stimulates the anterior pituitary gland to produce TSH <ref name="Brent" />. TSH binds to TSHR on the surface of thyroid cells and triggers the production of thyroid hormones thyroxine (T3) and triiodothyronine (T4) through G-protein coupled receptor (GPCR) signaling <ref name="Chu">Chu YD, Yeh CT. The Molecular Function and Clinical Role of Thyroid Stimulating Hormone Receptor in Cancer Cells. Cells. 2020;9(7):1730. [https://doi.org/10.3390/cells9071730 DOI:10.3390/cells9071730]</ref>. T3 and T4 circulate in the bloodstream and enter cells via thyroid hormone transporters to regulate metabolic functions. Additionally, T3 and T4 act in a negative feedback loop to inhibit further TSH production <ref name="Brent" />. | ||
| Line 14: | Line 14: | ||
== Structural Overview of TSHR == | == Structural Overview of TSHR == | ||
| - | There are three main domains of the Thyroid Stimulating Hormone Receptor. First is the <scene name='95/952703/Tmd/9'>Extracellular Domain</scene> shown in green. Region is concave in shape and is made up of primarily beta sheets and rich in Leucine. It is also called the leucine rich region. This is also the domain for key Lysine residues, which play a key role in binding. Second is the <scene name='95/952703/Tmd/10'>Transmembrane Domain</scene> shown in pink. This domain is made up of seven helices and undergoes a conformation change upon ligand binding that activates the GPCR signal cascade (GPCR is shown in yellow). The | + | There are three main domains of the Thyroid Stimulating Hormone Receptor. First is the <scene name='95/952703/Tmd/9'>Extracellular Domain</scene> shown in green. Region is concave in shape and is made up of primarily beta sheets and rich in Leucine. It is also called the leucine rich region <ref name="Kleinau">Kleinau G, Worth CL, Kreuchwig A, et al. Structural–Functional Features of the Thyrotropin Receptor: A Class A G-Protein-Coupled Receptor at Work. Frontiers in Endocrinology. 2017;8. Accessed April 2, 2023. [https://doi.org/10.3389/fendo.2017.00086 DOI: 10.3389/fendo.2017.00086]</ref>. This is also the domain for key Lysine residues, which play a key role in binding. Second is the <scene name='95/952703/Tmd/10'>Transmembrane Domain</scene> shown in pink. This domain is made up of seven helices and undergoes a conformation change upon ligand binding that activates the GPCR signal cascade (GPCR is shown in yellow) <ref name="Duan" />. The third region of the TSHR is the <scene name='95/952703/Tmd/11'>Hinge Region</scene> shown in orange. The Hinge Region plays a key role in the movement and stability of the TSHR. |
== TSHR Activation == | == TSHR Activation == | ||
| Line 39: | Line 39: | ||
== Ligand Binding == | == Ligand Binding == | ||
=== Binding of Thyroid Stimulating Hormone to TSHR=== | === Binding of Thyroid Stimulating Hormone to TSHR=== | ||
| - | The Thyroid Stimulating Hormone <scene name='95/952703/Tsh-ecd/3'>binds to the extracellular domain</scene> by complementary shape. The ECD and is curved and compliments the curvature of TSH similar to how a baseball fits into a glove. There are also several key ionic interactions between the TSH and TSHR. The key ionic interactions occurs in the <scene name='95/952703/Seatbelt/3'>Seat Belt region of TSH</scene> which is highlighted in yellow. The seatbelt region is located in the beta subunit of the TSH. <scene name='95/952703/Tsh-tshr_itxn-3/4'>The first ionic interaction</scene> is Glu118 from TSH and Lys58 from the ECD.<scene name='95/952703/Tsh-tshr_itxn-2/3'>The second interaction</scene> is between Asp111 from the TSH and Lys209 from the ECD. These interactions form salt bridges between the ECD and the TSH which allows for specificity of binding for TSH to TSHR. | + | The Thyroid Stimulating Hormone <scene name='95/952703/Tsh-ecd/3'>binds to the extracellular domain</scene> by complementary shape. The ECD and is curved and compliments the curvature of TSH similar to how a baseball fits into a glove. There are also several key ionic interactions between the TSH and TSHR. The key ionic interactions occurs in the <scene name='95/952703/Seatbelt/3'>Seat Belt region of TSH</scene> which is highlighted in yellow. The seatbelt region is located in the beta subunit of the TSH. <scene name='95/952703/Tsh-tshr_itxn-3/4'>The first ionic interaction</scene> is Glu118 from TSH and Lys58 from the ECD.<scene name='95/952703/Tsh-tshr_itxn-2/3'>The second interaction</scene> is between Asp111 from the TSH and Lys209 from the ECD. These interactions form salt bridges between the ECD and the TSH which allows for specificity of binding for TSH to TSHR <ref name="Duan" />,<ref name="Faust" />. |
| - | Other key interactions that allow for specificity of binding are <scene name='95/952703/Tsh-tshr_itxn-4/3'>polar and nonpolar interactions</scene> between the helix 1. Helix 1 contains several polar residues that interact with surrounding nonpolar residues like Leu62, Arg54, and Phe17. These interactions increase the activation potency and helps activate the push and pull mechanism of the hinge region. | + | |
| + | Other key interactions that allow for specificity of binding are <scene name='95/952703/Tsh-tshr_itxn-4/3'>polar and nonpolar interactions</scene> between the helix 1. Helix 1 contains several polar residues that interact with surrounding nonpolar residues like Leu62, Arg54, and Phe17. These interactions increase the activation potency and helps activate the push and pull mechanism of the hinge region <ref name="Duan" />,<ref name="Faust" />. | ||
=== Blocking TSHR in Active/Inactive States === | === Blocking TSHR in Active/Inactive States === | ||
[[Image:conformation1.png|400px|right|thumb|TSHR in active and inactive binding states. '''Left''' is TSH bound to TSHR. '''Middle''' is M22 bound to TSHR. '''Right''' is CS-17 bound to TSHR.]] | [[Image:conformation1.png|400px|right|thumb|TSHR in active and inactive binding states. '''Left''' is TSH bound to TSHR. '''Middle''' is M22 bound to TSHR. '''Right''' is CS-17 bound to TSHR.]] | ||
| - | The interactions between the ligand and the receptor have important consequences for disease states. In the image shown to the right are three different states of TSHR. The right-most structure is TSH bound to TSHR and is in it's upright active conformation. Comparing this is M22, shown in the middle, TSH binding offer not steric hinderance to keep it from being released. M22 can manifest with elevated levels of thyroid hormones which could be found in a person with Graves disease. M22 bound to TSHR is in the upright state and prevents transition to the down state because of the steric clash with the membrane which causes constitutive activation and symptoms of Graves disease. On the right most side is CS-17 bound to the TSHR. In contrast to TSH and M22 binding, CS-17 binds and locks TSHR in the down, inactive conformation. This prevents the signaling cascade to translation and causes constitutive inactivation. | + | The interactions between the ligand and the receptor have important consequences for disease states. In the image shown to the right are three different states of TSHR. The right-most structure is TSH bound to TSHR and is in it's upright active conformation. Comparing this is M22, shown in the middle, TSH binding offer not steric hinderance to keep it from being released. M22 can manifest with elevated levels of thyroid hormones which could be found in a person with Graves disease. M22 bound to TSHR is in the upright state and prevents transition to the down state because of the steric clash with the membrane which causes constitutive activation and symptoms of Graves disease. On the right most side is CS-17 bound to the TSHR. In contrast to TSH and M22 binding, CS-17 binds and locks TSHR in the down, inactive conformation. This prevents the signaling cascade to translation and causes constitutive inactivation <ref name="Faust" />. |
| - | These different ways to active and inactive TSHR could represent potential therapies for someone with graves disease or other thyroid related diseases with overacting TSH binding. Whereas current therapies target T3/T4 synthesis or destroy the gland using artificial hormones | + | |
| + | These different ways to active and inactive TSHR could represent potential therapies for someone with graves disease or other thyroid related diseases with overacting TSH binding. Whereas current therapies target T3/T4 synthesis or destroy the gland using artificial hormones, these diseases could instead be targeted with something like M22 or CS-17. | ||
== References == | == References == | ||
<references/> | <references/> | ||
Revision as of 23:35, 2 April 2023
| This Sandbox is Reserved from February 27 through August 31, 2023 for use in the course CH462 Biochemistry II taught by R. Jeremy Johnson at the Butler University, Indianapolis, USA. This reservation includes Sandbox Reserved 1765 through Sandbox Reserved 1795. |
To get started:
More help: Help:Editing |
| |||||||||||