|
m |
| Line 5: |
Line 5: |
| | | | |
| | == Introduction == | | == Introduction == |
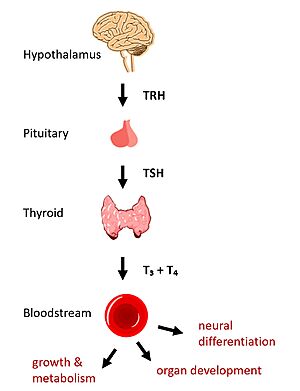
| - | [[Image:HPT Axis.jpg|300 px|right|thumb|Figure 1: TSHR on the surface of thyroid cells binds TSH ligand secreted by the anterior pituitary in the HPT signaling axis pathway, which regulates metabolism and growth.]] | + | [[Image:HPT Axis.jpg|300 px|right|thumb|Figure 1: TSHR binds TSH in the HPT signaling axis pathway, which regulates metabolism and growth.]] |
| - | In humans, the hypothalamic-pituitary-thyroid (HPT) signaling axis regulates functions including metabolism, growth, organ development, and neural differentiation <ref name="Brent">Brent GA. Mechanisms of thyroid hormone action. J Clin Invest. 2012;122(9):3035-3043. [https://doi.org/10.1172/JCI60047 DOI: 10.1172/JCI60047]</ref>. In this pathway, the thyroid stimulating hormone receptor (TSHR) activates transcription of thyroid hormones thyroxine (T3) and triiodothyronine (T4) in response to ligand binding by thyroid stimulating hormone (TSH). After a brief introduction to the biological significance of TSHR, this page explores the structure of TSHR and its significance to TSH binding and receptor activation. | + | In humans, the hypothalamic-pituitary-thyroid (HPT) signaling axis regulates functions including metabolism, growth, organ development, and neural differentiation <ref name="Brent">Brent GA. Mechanisms of thyroid hormone action. J Clin Invest. 2012;122(9):3035-3043. [https://doi.org/10.1172/JCI60047 DOI: 10.1172/JCI60047]</ref>. In this pathway, the thyroid stimulating hormone receptor (TSHR) activates transcription of thyroid hormones in response to ligand binding by thyroid stimulating hormone (TSH). After a brief introduction to the biological significance of TSHR, this page explores the structure of TSHR and its significance to TSH binding and receptor activation. |
| | | | |
| | == Biological Significance of TSHR == | | == Biological Significance of TSHR == |
| - | The HPT signaling axis involves the brain, thyroid gland, and bloodstream circulation. In the first step of the pathway, thyrotropin releasing hormone (TRH) is secreted by the hypothalamus, which in turn stimulates the anterior pituitary gland to produce TSH <ref name="Brent" />. TSH binds to TSHR on the surface of thyroid cells and triggers the production of T3 and T4 through through [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3967846/ G-protein coupled receptor (GPCR)] signaling <ref name="Chu">Chu YD, Yeh CT. The Molecular Function and Clinical Role of Thyroid Stimulating Hormone Receptor in Cancer Cells. Cells. 2020;9(7):1730. [https://doi.org/10.3390/cells9071730 DOI:10.3390/cells9071730]</ref>. T3 and T4 circulate in the bloodstream and enter cells via thyroid hormone transporters to regulate metabolic functions including organ development, neural differentiation, and growth and metabolism. Additionally, T3 and T4 act in a negative feedback loop to inhibit further TSH production <ref name="Brent" />. | + | The HPT signaling axis involves the brain, thyroid gland, and bloodstream circulation. In the first step of the pathway, thyrotropin releasing hormone (TRH) is secreted by the hypothalamus, which in turn stimulates the anterior pituitary gland to produce TSH <ref name="Brent" />. TSH binds to TSHR on the surface of thyroid cells and triggers the production of thyroid hormones thyroxine (T3) and triiodothyronine (T4) through [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3967846/ G-protein coupled receptor (GPCR)] signaling <ref name="Chu">Chu YD, Yeh CT. The Molecular Function and Clinical Role of Thyroid Stimulating Hormone Receptor in Cancer Cells. Cells. 2020;9(7):1730. [https://doi.org/10.3390/cells9071730 DOI:10.3390/cells9071730]</ref>. T3 and T4 circulate in the bloodstream and enter cells via thyroid hormone transporters to regulate metabolic functions. Additionally, T3 and T4 act in a negative feedback loop to inhibit further TSH production <ref name="Brent" />. |
| | | | |
| | Dysregulation of TSHR can lead to disease. In [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease#:~:text=Graves'%20disease%20is%20an%20autoimmune,the%20way%20your%20heart%20beats. Grave's disease], antibody analogs of TSH cause overactivation of TSHR, leading to clinical symptoms of hyperthyroidism <ref name="Chu" />. In contrast, congenital mutations which inactivate TSHR can lead to hypothyroidism, which results in growth retardation and neurologic impairment if left untreated <ref name="Brent" />. | | Dysregulation of TSHR can lead to disease. In [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease#:~:text=Graves'%20disease%20is%20an%20autoimmune,the%20way%20your%20heart%20beats. Grave's disease], antibody analogs of TSH cause overactivation of TSHR, leading to clinical symptoms of hyperthyroidism <ref name="Chu" />. In contrast, congenital mutations which inactivate TSHR can lead to hypothyroidism, which results in growth retardation and neurologic impairment if left untreated <ref name="Brent" />. |
| | | | |
| - | == Significance of TSHR Structure to Signaling Activation == | + | == Structural Overview of TSHR == |
| - | === Domains of TSHR Contribute to Signaling ===
| + | There are three main domains of the thyroid stimulating hormone receptor. First is the <scene name='95/952703/Tmd/9'>extracellular domain</scene> shown in green, which is concave in shape. It is also called the leucine rich region because it is made primarily of beta sheets which are rich in leucine <ref name="Kleinau">Kleinau G, Worth CL, Kreuchwig A, et al. Structural–Functional Features of the Thyrotropin Receptor: A Class A G-Protein-Coupled Receptor at Work. Frontiers in Endocrinology. 2017;8. Accessed April 2, 2023. [https://doi.org/10.3389/fendo.2017.00086 DOI: 10.3389/fendo.2017.00086]</ref>. This domain also contains lysine residues which play a key role in binding. Second is the <scene name='95/952703/Tmd/10'>transmembrane domain</scene> shown in pink. This domain is made up of seven helices and undergoes a conformation change upon ligand binding that activates the GPCR signal cascade <ref name="Duan" />. The third region of the TSHR is the <scene name='95/952703/Tmd/11'>hinge region</scene> shown in orange. The hinge region plays a key role in the movement and stability of the TSHR. |
| - | There are three main domains of the thyroid stimulating hormone receptor, each of which plays a distinct role in signaling activation. First is the <scene name='95/952703/Tmd/9'>extracellular domain</scene>, which is concave in shape. It is also called the leucine rich region because it is made primarily of beta sheets which are rich in leucine <ref name="Kleinau">Kleinau G, Worth CL, Kreuchwig A, et al. Structural–Functional Features of the Thyrotropin Receptor: A Class A G-Protein-Coupled Receptor at Work. Frontiers in Endocrinology. 2017;8. Accessed April 2, 2023. [https://doi.org/10.3389/fendo.2017.00086 DOI: 10.3389/fendo.2017.00086]</ref>. This domain also contains lysine residues which play a key role in TSH binding. Second is the <scene name='95/952703/Tmd/10'>transmembrane domain</scene> composed of seven alpha helices. The TMD undergoes a conformation change upon ligand binding that activates the intracellular GPCR signal cascade <ref name="Duan" />. The third region of the TSHR is the <scene name='95/952703/Tmd/11'>hinge region</scene> shown in orange. The hinge region controls the movement and stability of the TSHR. Specifically, the hinge region allows the receptor to undergo a conformation change which turns the signaling pathway on and off, the details of which are discussed in the proceeding section. | + | |
| | | | |
| - | === Hinge Motion Controls Signaling Activation === | + | == TSHR Activation == |
| - | The TSHR exists in two states: <scene name='95/952702/Overlay/2'>active and inactive </scene>. When the extracellular domain is hinged down, the receptor is inactive and no signaling activation occurs. Upward movement of the ECD into the active states pulls on the transmembrane helices to activate the G-protein, which in turns set off an intracellular signaling cascade that ends in transcriptional activation of thyroid hormones, including T3 and T4 (Fig. __).
| + | === Hinge Motion === |
| | + | Central to the biological function of TSHR is its hinge motion which allows for transition between the <scene name='95/952702/Overlay/2'>active and inactive states</scene>. Deformation of the hinge region accommodates up-and-down rotation of the extracellular domain as a rigid body about an imaginary 55 degree axis. When the extracellular domain is upright, the receptor actively signals for thyroid hormone production. When the extracellular domain is hinged down, the receptor is inactive and no signaling activation occurs. Notably, transition between the two states occurs spontaneously; favoring of the active or inactive conformation is influenced by hinge interactions and ligand binding <ref name="Faust">PMID:35940205</ref>. |
| | | | |
| - | The hinge motion of the TSHR is made possible by the hinge region structure. Deformation of the hinge region accommodates up-and-down rotation of the extracellular domain as a rigid body, which hinges approximately 55 degrees around an imaginary axis <ref name="Faust">PMID:35940205</ref>. As the receptor transitions towards its active state, stretching of the hinge region leads to shifting of the transmembrane helices. Additionally, the hinge region itself serves as an agonist of TSHR activation through intermolecular interactions with the transmembrane domain in the active state. While switching between the active and inactive states is spontaneous, these hinge interactions favor the active conformation, as does binding of the TSH ligand <ref name="Faust">PMID:35940205</ref>. To fully understand these stabilizing interactions, a deeper discussion of hinge region anatomy is warranted.
| + | Two observations help to explain how hinging of the extracellular domain can lead to signaling activation: |
| | + | #Slinky-like deformation of the hinge region shifts the <scene name='95/952702/P10_movement/2'>N-terminus of the p10</scene> region 5 Angstroms over the course of the movement <ref name="Faust" />. |
| | + | #Stretching of the hinge pulls on the linked helices in the transmembrane domain, shifting <scene name='95/952702/Helix7_movement/2'>helix 7</scene> about 4 Angstroms inward <ref name="Faust" />. |
| | + | An animation of the hinge motion can be viewed here: [[Image:TSHR_MorphBetterAngle.mp4|Figure 1]]. |
| | | | |
| - | [[Image:TSHR_MorphBetterAngle_GIF.gif|thumb|right|Figure 2: Hinge region (blue) accomondates rigid movement of the ECD (green) towards and away from the TMD (pink). ]].
| + | === Stabilizing Interactions in the Hinge === |
| - | | + | To understand stabilizing interactions which accommodate the hinge motion, the hinge region can be subdivided into the <scene name='95/952702/Hinge_helix_intro/3'>hinge helix</scene>, which lies at the intersection of the extracellular and transmembrane domains; <scene name='95/952702/Helix_1_intro/5'>helix 1</scene>, which sticks up and serves as a binding platform for the TSH ligand; the <scene name='95/952702/Linker_intro/4'>linker</scene> region, which connects helix 1 with the p10 region; and the <scene name='95/952702/P10_intro/2'>p10</scene> region, a conserved 10-amino acid sequence which connects to transmembrane helix 7 and undergoes most of the deformation <ref name="Faust" /> <ref name="Duan">PMID:35940204</ref>. |
| - | === Stabilizing Interactions in the Hinge Favor Signaling Activation === | + | |
| - | The hinge region can be subdivided into the <scene name='95/952702/Hinge_helix_intro/3'>hinge helix</scene>, which lies at the intersection of the extracellular and transmembrane domains; <scene name='95/952702/Helix_1_intro/5'>helix 1</scene>, which sticks up and serves as a binding platform for the TSH ligand; the <scene name='95/952702/Linker_intro/4'>linker</scene> region, which connects helix 1 with the p10 region; and the <scene name='95/952702/P10_intro/2'>p10</scene> region, a conserved 10-amino acid sequence which connects to transmembrane helix 7 and undergoes most of the deformation <ref name="Faust" /> <ref name="Duan">PMID:35940204</ref>.
| + | |
| | | | |
| | Two key disulfide bridges within the hinge region help to maintain its structure and orientation <ref name="Duan" />. | | Two key disulfide bridges within the hinge region help to maintain its structure and orientation <ref name="Duan" />. |
| Line 31: |
Line 32: |
| | #The <scene name='95/952702/Linker_hinge_disulfide/3'>second disulfide bridge</scene> connects the hinge helix with the p10 region. | | #The <scene name='95/952702/Linker_hinge_disulfide/3'>second disulfide bridge</scene> connects the hinge helix with the p10 region. |
| | | | |
| - | Interactions with the EC and TM domains help to stabilize the hinge in the upright, active conformation <ref name="Faust" />.
| + | The upright, active conformation of the hinge is stabilized by its respective interactions with the EC and TM domains <ref name="Faust" />. |
| | #A <scene name='95/952702/Hydrophobic_interaction/2'>hydrophobic interaction</scene> occurs between Y279 in the hinge helix and I486 in EC loop region 1, which protrudes from the TM helices. | | #A <scene name='95/952702/Hydrophobic_interaction/2'>hydrophobic interaction</scene> occurs between Y279 in the hinge helix and I486 in EC loop region 1, which protrudes from the TM helices. |
| - | #An <scene name='95/952702/Ionic_interaction/3'>ionic interaction</scene> occurs between K660 in TM helix 7 and E409 in the p10 region. | + | #An <scene name='95/952702/Ionic_interaction/3'>ionic interaction</scene> occurs between K660 in TM helix 7 and E409 in the p10 region. |
| - | | + | |
| - | Two observations help to explain how hinging of the extracellular domain can lead to signaling activation:
| + | |
| - | #Slinky-like deformation of the hinge region shifts the <scene name='95/952702/P10_movement/3'>N-terminus of the p10</scene> region 5 Angstroms over the course of the movement <ref name="Faust" />.
| + | |
| - | #Stretching of the hinge pulls on the linked helices in the transmembrane domain, shifting <scene name='95/952702/Helix7_movement/2'>helix 7</scene> about 4 Angstroms inward <ref name="Faust" />.
| + | |
| | | | |
| - | If these stabilizing interactions are disrupted, TSHR function is affected. For instance, the mutation I496F has been observed to cause constitutive receptor activation and decreased sensitivity to the TSH ligand, suggesting that the bulkier phenylalanine overly stabilizes the <scene name='95/952702/Hydrophobic_interaction/2'>hydrophobic interaction</scene>, leading to overactivation <ref name="Faust" />. Contrastingly, TSHR underactivation results from disrupting the <scene name='95/952702/Ionic_interaction/3'>ionic interaction</scene> with an E409A mutation, which is associated with diminished receptor activation and TSH potency <ref name="Faust" />. | + | If the stabilizing interactions are disrupted, TSHR function is affected. For instance, the mutation I496F has been observed to cause constitutive receptor activation and decreased sensitivity to the TSH ligand, suggesting that the bulkier phenylalanine strengthens the hydrophobic interaction too much, leading to overactivation. Contrastingly, TSHR underactivation results from disrupting the ionic interaction with an E409A mutation, which is associated with diminished receptor activation and TSH potency <ref name="Faust" />. |
| | | | |
| - | == Significance of TSHR Structure to Ligand Binding == | + | == Ligand Binding == |
| - | === Binding of Thyroid Stimulating Hormone to TSHR === | + | === Binding of Thyroid Stimulating Hormone to TSHR=== |
| | The thyroid stimulating hormone <scene name='95/952703/Tsh-ecd/3'>binds to the extracellular domain</scene> by complementary shape. The ECD is curved and compliments the curvature of TSH similar to how a baseball fits into a glove. There are also several key ionic interactions between the TSH and TSHR. The key ionic interactions occur in the <scene name='95/952703/Seatbelt/3'>seat belt region of TSH</scene> which is highlighted in yellow. The seatbelt region is located in the beta subunit of the TSH. <scene name='95/952703/Tsh-tshr_itxn-3/4'>The first ionic interaction</scene> is Glu118 from TSH and Lys58 from the ECD.<scene name='95/952703/Tsh-tshr_itxn-2/3'>The second interaction</scene> is between Asp111 from the TSH and Lys209 from the ECD. These interactions form salt bridges between the ECD and the TSH which allows for specificity of binding for TSH to TSHR <ref name="Duan" />,<ref name="Faust" />. | | The thyroid stimulating hormone <scene name='95/952703/Tsh-ecd/3'>binds to the extracellular domain</scene> by complementary shape. The ECD is curved and compliments the curvature of TSH similar to how a baseball fits into a glove. There are also several key ionic interactions between the TSH and TSHR. The key ionic interactions occur in the <scene name='95/952703/Seatbelt/3'>seat belt region of TSH</scene> which is highlighted in yellow. The seatbelt region is located in the beta subunit of the TSH. <scene name='95/952703/Tsh-tshr_itxn-3/4'>The first ionic interaction</scene> is Glu118 from TSH and Lys58 from the ECD.<scene name='95/952703/Tsh-tshr_itxn-2/3'>The second interaction</scene> is between Asp111 from the TSH and Lys209 from the ECD. These interactions form salt bridges between the ECD and the TSH which allows for specificity of binding for TSH to TSHR <ref name="Duan" />,<ref name="Faust" />. |
| | | | |
| Line 49: |
Line 46: |
| | === Blocking TSHR in Active/Inactive States === | | === Blocking TSHR in Active/Inactive States === |
| | [[Image:conformation1.png|400px|right|thumb|'''Figure 2''' TSHR in active and inactive binding states. '''Left''' is TSH bound to TSHR. '''Middle''' is M22 bound to TSHR. '''Right''' is CS-17 bound to TSHR.]] | | [[Image:conformation1.png|400px|right|thumb|'''Figure 2''' TSHR in active and inactive binding states. '''Left''' is TSH bound to TSHR. '''Middle''' is M22 bound to TSHR. '''Right''' is CS-17 bound to TSHR.]] |
| - | The interactions between the ligand and the receptor have important consequences for disease states. In the image shown to the right are three different states of TSHR. The left-most structure is TSH bound to TSHR in the upright active conformation. In contrast to the native TSH conformation, [https://www.creativebiolabs.net/Anti-TSHR-Antibody-24960.htm M22] bound to TSHR (middle) locks the receptor in the upright state and prevents transition to the down state because of steric clash with the membrane. This conformation causes constitutive activation and the elevated levels of thyroid hormones which are found in a person with Grave's disease. On the right-most side is [https://pubmed.ncbi.nlm.nih.gov/19299457/ CS-17] bound to the TSHR. In contrast to TSH and M22 binding, CS-17 binds and locks TSHR in the down, inactive conformation. This prevents the signaling cascade to translation and causes constitutive inactivation <ref name="Faust" />. | + | The interactions between the ligand and the receptor have important consequences for disease states. In the image shown to the right are three different states of TSHR. The left-most structure is TSH bound to TSHR in the upright active conformation. In the middle receptor-ligand pair, [https://www.creativebiolabs.net/Anti-TSHR-Antibody-24960.htm M22] is bound to TSHR is in the upright state and prevents transition to the down state because of steric clash with the membrane. This conformation causes constitutive activation and the elevated levels of thyroid hormones which are found in a person with Grave's disease. On the right-most side is [https://pubmed.ncbi.nlm.nih.gov/19299457/ CS-17] bound to the TSHR. In contrast to TSH and M22 binding, CS-17 binds and locks TSHR in the down, inactive conformation. This prevents the signaling cascade to translation and causes constitutive inactivation <ref name="Faust" />. |
| | | | |
| | These different ways to active and inactive TSHR could represent potential therapies for someone with Grave's disease or other thyroid-related diseases with overactive TSH binding. Whereas current therapies target T3/T4 synthesis or destroy the gland using artificial hormones, these diseases could instead be targeted with something like CS-17 which would compete with M22 and TSH to lessen overactivation. | | These different ways to active and inactive TSHR could represent potential therapies for someone with Grave's disease or other thyroid-related diseases with overactive TSH binding. Whereas current therapies target T3/T4 synthesis or destroy the gland using artificial hormones, these diseases could instead be targeted with something like CS-17 which would compete with M22 and TSH to lessen overactivation. |
|
Thyroid Stimulating Hormone Receptor (TSHR) Structure and Function
Introduction
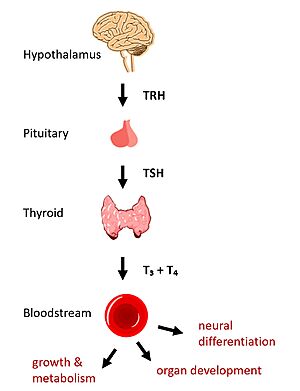 Figure 1: TSHR binds TSH in the HPT signaling axis pathway, which regulates metabolism and growth. In humans, the hypothalamic-pituitary-thyroid (HPT) signaling axis regulates functions including metabolism, growth, organ development, and neural differentiation [1]. In this pathway, the thyroid stimulating hormone receptor (TSHR) activates transcription of thyroid hormones in response to ligand binding by thyroid stimulating hormone (TSH). After a brief introduction to the biological significance of TSHR, this page explores the structure of TSHR and its significance to TSH binding and receptor activation.
Biological Significance of TSHR
The HPT signaling axis involves the brain, thyroid gland, and bloodstream circulation. In the first step of the pathway, thyrotropin releasing hormone (TRH) is secreted by the hypothalamus, which in turn stimulates the anterior pituitary gland to produce TSH [1]. TSH binds to TSHR on the surface of thyroid cells and triggers the production of thyroid hormones thyroxine (T3) and triiodothyronine (T4) through G-protein coupled receptor (GPCR) signaling [2]. T3 and T4 circulate in the bloodstream and enter cells via thyroid hormone transporters to regulate metabolic functions. Additionally, T3 and T4 act in a negative feedback loop to inhibit further TSH production [1].
Dysregulation of TSHR can lead to disease. In Grave's disease, antibody analogs of TSH cause overactivation of TSHR, leading to clinical symptoms of hyperthyroidism [2]. In contrast, congenital mutations which inactivate TSHR can lead to hypothyroidism, which results in growth retardation and neurologic impairment if left untreated [1].
Structural Overview of TSHR
There are three main domains of the thyroid stimulating hormone receptor. First is the shown in green, which is concave in shape. It is also called the leucine rich region because it is made primarily of beta sheets which are rich in leucine [3]. This domain also contains lysine residues which play a key role in binding. Second is the shown in pink. This domain is made up of seven helices and undergoes a conformation change upon ligand binding that activates the GPCR signal cascade [4]. The third region of the TSHR is the shown in orange. The hinge region plays a key role in the movement and stability of the TSHR.
TSHR Activation
Hinge Motion
Central to the biological function of TSHR is its hinge motion which allows for transition between the . Deformation of the hinge region accommodates up-and-down rotation of the extracellular domain as a rigid body about an imaginary 55 degree axis. When the extracellular domain is upright, the receptor actively signals for thyroid hormone production. When the extracellular domain is hinged down, the receptor is inactive and no signaling activation occurs. Notably, transition between the two states occurs spontaneously; favoring of the active or inactive conformation is influenced by hinge interactions and ligand binding [5].
Two observations help to explain how hinging of the extracellular domain can lead to signaling activation:
- Slinky-like deformation of the hinge region shifts the region 5 Angstroms over the course of the movement [5].
- Stretching of the hinge pulls on the linked helices in the transmembrane domain, shifting about 4 Angstroms inward [5].
An animation of the hinge motion can be viewed here: Image:TSHR MorphBetterAngle.mp4.
Stabilizing Interactions in the Hinge
To understand stabilizing interactions which accommodate the hinge motion, the hinge region can be subdivided into the , which lies at the intersection of the extracellular and transmembrane domains; , which sticks up and serves as a binding platform for the TSH ligand; the region, which connects helix 1 with the p10 region; and the region, a conserved 10-amino acid sequence which connects to transmembrane helix 7 and undergoes most of the deformation [5] [4].
Two key disulfide bridges within the hinge region help to maintain its structure and orientation [4].
- The connects the hinge helix with the linker region
- The connects the hinge helix with the p10 region.
The upright, active conformation of the hinge is stabilized by its respective interactions with the EC and TM domains [5].
- A occurs between Y279 in the hinge helix and I486 in EC loop region 1, which protrudes from the TM helices.
- An occurs between K660 in TM helix 7 and E409 in the p10 region.
If the stabilizing interactions are disrupted, TSHR function is affected. For instance, the mutation I496F has been observed to cause constitutive receptor activation and decreased sensitivity to the TSH ligand, suggesting that the bulkier phenylalanine strengthens the hydrophobic interaction too much, leading to overactivation. Contrastingly, TSHR underactivation results from disrupting the ionic interaction with an E409A mutation, which is associated with diminished receptor activation and TSH potency [5].
Ligand Binding
Binding of Thyroid Stimulating Hormone to TSHR
The thyroid stimulating hormone by complementary shape. The ECD is curved and compliments the curvature of TSH similar to how a baseball fits into a glove. There are also several key ionic interactions between the TSH and TSHR. The key ionic interactions occur in the which is highlighted in yellow. The seatbelt region is located in the beta subunit of the TSH. is Glu118 from TSH and Lys58 from the ECD. is between Asp111 from the TSH and Lys209 from the ECD. These interactions form salt bridges between the ECD and the TSH which allows for specificity of binding for TSH to TSHR [4],[5].
Other key interactions that allow for specificity of binding are between TSH and helix 1. Helix 1 contains several polar residues that interact with surrounding nonpolar residues like Leu62 and Phe17. Positively charged Arg54 was also seen to interact with Helix 1. These interactions increase the activation potency and help activate the push and pull mechanism of the hinge region [4],[5].
Blocking TSHR in Active/Inactive States
 Figure 2 TSHR in active and inactive binding states. Left is TSH bound to TSHR. Middle is M22 bound to TSHR. Right is CS-17 bound to TSHR. The interactions between the ligand and the receptor have important consequences for disease states. In the image shown to the right are three different states of TSHR. The left-most structure is TSH bound to TSHR in the upright active conformation. In the middle receptor-ligand pair, M22 is bound to TSHR is in the upright state and prevents transition to the down state because of steric clash with the membrane. This conformation causes constitutive activation and the elevated levels of thyroid hormones which are found in a person with Grave's disease. On the right-most side is CS-17 bound to the TSHR. In contrast to TSH and M22 binding, CS-17 binds and locks TSHR in the down, inactive conformation. This prevents the signaling cascade to translation and causes constitutive inactivation [5].
These different ways to active and inactive TSHR could represent potential therapies for someone with Grave's disease or other thyroid-related diseases with overactive TSH binding. Whereas current therapies target T3/T4 synthesis or destroy the gland using artificial hormones, these diseases could instead be targeted with something like CS-17 which would compete with M22 and TSH to lessen overactivation.
References
- ↑ 1.0 1.1 1.2 1.3 Brent GA. Mechanisms of thyroid hormone action. J Clin Invest. 2012;122(9):3035-3043. DOI: 10.1172/JCI60047
- ↑ 2.0 2.1 Chu YD, Yeh CT. The Molecular Function and Clinical Role of Thyroid Stimulating Hormone Receptor in Cancer Cells. Cells. 2020;9(7):1730. DOI:10.3390/cells9071730
- ↑ Kleinau G, Worth CL, Kreuchwig A, et al. Structural–Functional Features of the Thyrotropin Receptor: A Class A G-Protein-Coupled Receptor at Work. Frontiers in Endocrinology. 2017;8. Accessed April 2, 2023. DOI: 10.3389/fendo.2017.00086
- ↑ 4.0 4.1 4.2 4.3 4.4 Duan J, Xu P, Luan X, Ji Y, He X, Song N, Yuan Q, Jin Y, Cheng X, Jiang H, Zheng J, Zhang S, Jiang Y, Xu HE. Hormone- and antibody-mediated activation of the thyrotropin receptor. Nature. 2022 Aug 8. pii: 10.1038/s41586-022-05173-3. doi:, 10.1038/s41586-022-05173-3. PMID:35940204 doi:http://dx.doi.org/10.1038/s41586-022-05173-3
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 Faust B, Billesbolle CB, Suomivuori CM, Singh I, Zhang K, Hoppe N, Pinto AFM, Diedrich JK, Muftuoglu Y, Szkudlinski MW, Saghatelian A, Dror RO, Cheng Y, Manglik A. Autoantibody mimicry of hormone action at the thyrotropin receptor. Nature. 2022 Aug 8. pii: 10.1038/s41586-022-05159-1. doi:, 10.1038/s41586-022-05159-1. PMID:35940205 doi:http://dx.doi.org/10.1038/s41586-022-05159-1
|