We apologize for Proteopedia being slow to respond. For the past two years, a new implementation of Proteopedia has been being built. Soon, it will replace this 18-year old system. All existing content will be moved to the new system at a date that will be announced here.
Sandbox Reserved 1780
From Proteopedia
(Difference between revisions)
| Line 5: | Line 5: | ||
=== Active and Inactive Form === | === Active and Inactive Form === | ||
[[Image:Morph_pics2.png|200 px|right|thumb|Figure 2: Inactive form of the thyrotropin receptor shown in blue. Active form of the thyrotropin receptor shown in green.]] | [[Image:Morph_pics2.png|200 px|right|thumb|Figure 2: Inactive form of the thyrotropin receptor shown in blue. Active form of the thyrotropin receptor shown in green.]] | ||
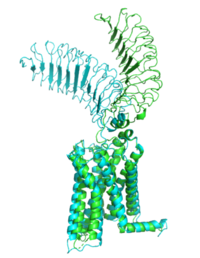
| - | The TSHR protein exists in two states: active and inactive (Figure 2) | + | The TSHR protein exists in two states: active and inactive (Figure 2). The <scene name='95/952708/Tshr_chainr/4'>TSHR active form</scene> exists when bound to the <scene name='95/952708/Tsh_7t9i/1'>TSH</scene>. One proposed mechanism for the transition from the active to inactive describes that in a natural state, the TSHR ECD can spontaneously transition to the up state, leading to constitutive activity. In this active state, TSH will bind and keep the active state in the up position because of clash with the cell membrane.<ref name="Faust" /> Conformational change of ECD allows for signal transduction through the TM and into the cell. The ECD rotates 55 degrees up in the active form. <ref name="Faust" /> |
== TSHR Agonists and Antagonists == | == TSHR Agonists and Antagonists == | ||
| - | Chemical [https://en.wikipedia.org/wiki/Agonist agonists] are found in many living systems and serve as a way to activate receptors or pathways that are necessary for a wide array of biological processes. Chemical [https://en.wikipedia.org/wiki/Receptor_antagonist antagonists] block or inhibit biological processes. Different types of agonists/antagonists exist within the body including hormones, antibodies, and neurotransmitters. The body naturally produces autoantibodies that can act as agonists and mimic the activating mechanism of the natural hormone. | + | Chemical [https://en.wikipedia.org/wiki/Agonist agonists] are found in many living systems and serve as a way to activate receptors or pathways that are necessary for a wide array of biological processes. Chemical [https://en.wikipedia.org/wiki/Receptor_antagonist antagonists] block or inhibit biological processes. Different types of agonists/antagonists exist within the body including hormones, antibodies, and neurotransmitters. The body naturally produces autoantibodies that can act as agonists and mimic the activating mechanism of the natural hormone.<ref name="Miguel"> doi:10.1677/JME-08-0152</ref>. |
===M22 Agonist=== | ===M22 Agonist=== | ||
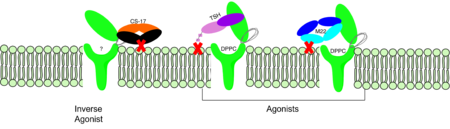
| - | <scene name='95/952708/M22_edited/3'>M22</scene> is a [https://en.wikipedia.org/wiki/Monoclonal_antibody monoclonal antibody] that was isolated from a patient with [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease Graves' Disease]. In Graves' disease, | + | <scene name='95/952708/M22_edited/3'>M22</scene> is a [https://en.wikipedia.org/wiki/Monoclonal_antibody monoclonal antibody] that was isolated from a patient with [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease Graves' Disease]. In Graves' disease, autoantibodies mimic TSH function and cause thyroid overactivity. <ref name="Miguel"> doi:10.1677/JME-08-0152</ref>. The M22 [https://en.wikipedia.org/wiki/Autoantibody autoantibody] activates TSHR by causing a membrane clash with the ECD and cell membrane, keeping the TSHR in the active state by preventing the TSHR from rotating to the inactive state (Figure 3). M22 mimics TSH activation of TSHR because it is a potent activator for TSHR. <ref name="Faust"> DOI:10.1038/s41586-022-05159-1</ref> Although M22 binds in a similar manner to TSH, M22 does not interact with the hinge region when bound to TSHR, whereas TSH bound to TSHR does.<ref name="Faust"> DOI:10.1038/s41586-022-05159-1</ref> This finding shows that the hinge region is not necessary for the activation of TSHR, and leads to the discovery of other methods of activation. [[Image:Agonist pic.png|450 px|right|thumb|Figure 3: Agonist and antagonist drugs for activating or inactivating the TSHR protein.]] |
===CS-17 Inverse Agonist=== | ===CS-17 Inverse Agonist=== | ||
| Line 20: | Line 20: | ||
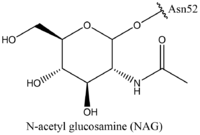
Thyroid-stimulating hormone <scene name='95/952708/Tsh_7t9i/1'>(TSH)</scene>, as previously mentioned, is a hormone that stimulates the thyroid gland to produce proteins that are vital for many metabolic pathways in the body's tissue. TSH activates the TSHR protein by binding to the concave surface of the LRRD and hinge region to keep TSHR in its active state by clashing with the membrane <ref name="Duan"> DOI:10.1038/s41586-022-05173-3</ref>. (Figure 3). This clash is caused by glycosylations of an N52 residue on the <scene name='95/952707/Tsh_7t9i/1'>alpha subunit of TSH</scene>. These modifications to the N residue are N-acetyl glucosamine modifications (Figure 4). They stick out from the alpha subunit of TSH to clash with the cell membrane and keep TSH in the active state. | Thyroid-stimulating hormone <scene name='95/952708/Tsh_7t9i/1'>(TSH)</scene>, as previously mentioned, is a hormone that stimulates the thyroid gland to produce proteins that are vital for many metabolic pathways in the body's tissue. TSH activates the TSHR protein by binding to the concave surface of the LRRD and hinge region to keep TSHR in its active state by clashing with the membrane <ref name="Duan"> DOI:10.1038/s41586-022-05173-3</ref>. (Figure 3). This clash is caused by glycosylations of an N52 residue on the <scene name='95/952707/Tsh_7t9i/1'>alpha subunit of TSH</scene>. These modifications to the N residue are N-acetyl glucosamine modifications (Figure 4). They stick out from the alpha subunit of TSH to clash with the cell membrane and keep TSH in the active state. | ||
| - | + | ||
Revision as of 20:21, 10 April 2023
| This Sandbox is Reserved from February 27 through August 31, 2023 for use in the course CH462 Biochemistry II taught by R. Jeremy Johnson at the Butler University, Indianapolis, USA. This reservation includes Sandbox Reserved 1765 through Sandbox Reserved 1795. |
To get started:
More help: Help:Editing |
| |||||||||||
References
- ↑ 1.0 1.1 1.2 1.3 Faust B, Billesbolle CB, Suomivuori CM, Singh I, Zhang K, Hoppe N, Pinto AFM, Diedrich JK, Muftuoglu Y, Szkudlinski MW, Saghatelian A, Dror RO, Cheng Y, Manglik A. Autoantibody mimicry of hormone action at the thyrotropin receptor. Nature. 2022 Aug 8. pii: 10.1038/s41586-022-05159-1. doi:, 10.1038/s41586-022-05159-1. PMID:35940205 doi:http://dx.doi.org/10.1038/s41586-022-05159-1
- ↑ 2.0 2.1 Nunez Miguel R, Sanders J, Chirgadze DY, Furmaniak J, Rees Smith B. Thyroid stimulating autoantibody M22 mimics TSH binding to the TSH receptor leucine rich domain: a comparative structural study of protein-protein interactions. J Mol Endocrinol. 2009 May;42(5):381-95. Epub 2009 Feb 16. PMID:19221175 doi:10.1677/JME-08-0152
- ↑ 3.0 3.1 Chen, C.-R., McLachlan, S. M., & Rapoport, B. (2007). Suppression of thyrotropin receptor constitutive activity by a monoclonal antibody with inverse agonist activity. Endocrinology, 148(5), 2375–2382. https://doi.org/10.1210/en.2006-1754
- ↑ Duan J, Xu P, Luan X, Ji Y, He X, Song N, Yuan Q, Jin Y, Cheng X, Jiang H, Zheng J, Zhang S, Jiang Y, Xu HE. Hormone- and antibody-mediated activation of the thyrotropin receptor. Nature. 2022 Aug 8. pii: 10.1038/s41586-022-05173-3. doi:, 10.1038/s41586-022-05173-3. PMID:35940204 doi:http://dx.doi.org/10.1038/s41586-022-05173-3