Introduction
Sodium-taurocholate Co-transporting Polypeptide (NTCP) is a member of the solute carrier membrane transport protein family. It is found within the membrane of
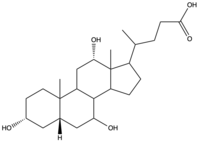
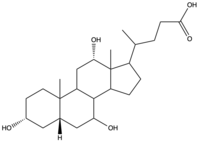
Figure 1. Structure of
Cholic Acid, an example of a bile acid.
, and its primary role is to facilitate the transport of
bile salts into hepatocytes from the bloodstream (Figure 1).
[1] This is important because 90% of human bile salts are recycled daily, so the function of NTCP is critical in providing bile acids to solubilize fats for digestion. In addition to transporting bile acids into the cytoplasm of hepatocytes, NTCP also serves as an entry point receptor for
Hepatitis B (HBV) and
Hepatitis D (HDV) viruses (Figure 2).
[2] 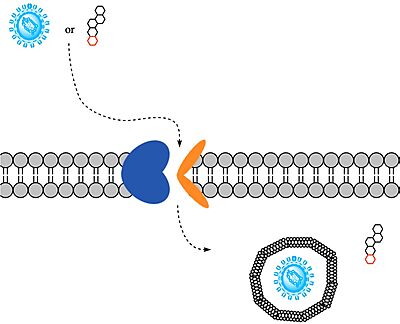
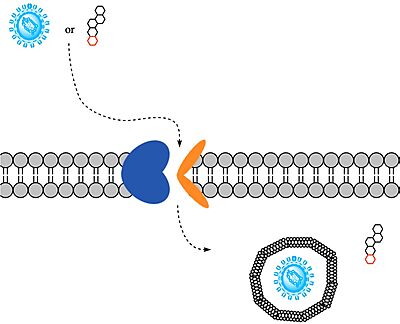
Figure 2. Overall NTCP mechanism. Bile salts and HBV/HDV
viruses bind to NTCP. NTCP transports bile salts through an inner pore, releasing the bile salt into the cytoplasm. Transport of viral particles occurs via endocytosis of NTCP.
Structure
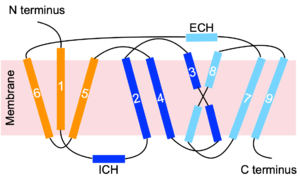
NTCP is a transmembrane protein found in hepatocyte cells. It consists of nine , with the N-terminus located on the extracellular side of the plasma membrane and the C-terminus located on the intracellular side (Figure 3). The transmembrane helices are connected by short loops as well as extracellular and intracellular alpha helices that lie nearly parallel to the membrane.[2] Structures of NTCP were determined by cryogenic electron microscopy (Cryo-EM) of NTCP in complex with antibodies or nanobodies, which served to stabilize two known conformational states of NTCP. [1] [2] [3] [4] These complexed antibodies/nanobodies have been removed from all structures shown on this page.
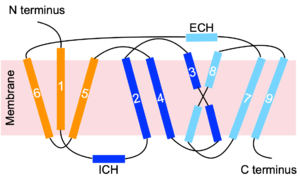
Figure 3. NTCP topology. Transmembrane helices are numbered. The panel domain is shown in orange. The core domain is shown in two shades of blue. Light and dark blue shades represent different helix bundles of the core domain, which together demonstrate pseudo two-fold symmetry.
Domains
NTCP contains : the core and panel domains (Figure 3). Movement of these two domains allows recognition and transport of bile acids into hepatocytes.
- Panel Domain:
- Formed by transmembrane helices TM1, TM5, and TM6.
- Core domain:
- Formed by the packing of a helix bundle of TM2, TM3, and TM4 with another helix bundle of TM7, TM8, and TM9 (Figure 3). These are related by pseudo two-fold symmetry.[5]
Proline/Glycine Hinge
in the and (Figure 3) act as hinges between the and in the mechanism of bile salt uptake. This flexibility allows separation of the core and panel domains, creating a pore open to the extracellular space and exposing critical Na+ binding sites. Once substrate binds the open-pore state, this hinge allows the transition to close this pore relative to the extracellular side and open to the cytoplasmic side, thus allowing release of substrate into the cell.[1]
Sodium Binding Sites
To transport a single bile salt from the blood to the cytoplasm of the hepatocyte, must bind to NTCP in the open-pore state, using two .[4] The residues in the include S105, N106, T123, and E257. The residues in the include Q68 and Q261. Mutations to these significant residues inhibit the binding of sodium ions, and consequently, inhibit the transport of bile salts by NTCP.[4] Secondary active transport is used, as the transport of bile acids into the cell is thermodynamically unfavorable, but is coupled with the favorable transport of two sodium into into the cell to make the overall process thermodynamically favorable.[1] When the bile salts are released into the cell, NTCP transitions to the , where the pore is now closed to the extracellular side.
Function
Mechanism of Bile Salt Uptake
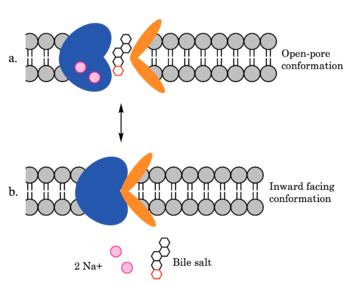
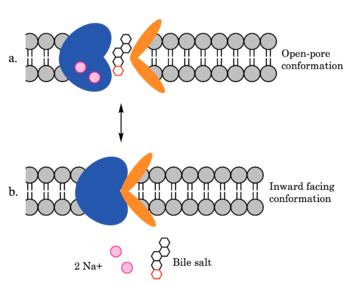
Figure 4. Mechanism of bile salt uptake by NTCP. A bile salt and two Na+ ions bind to NTCP in the open-pore state. Transition to the inward-facing state allows release of the bile salt and ions into the cytoplasm.
NTCP utilizes secondary active transport to uptake bile salts from blood plasma into the cytoplasm of liver cells (Figure 4). The transport of one bile salt is driven by the downhill transport of 2 Na+ ions along sodium’s electrochemical gradient. Two bile salts and two Na+ ions bind to the (Figure 4a), but only one bile salt (along with two Na+ ions) is released into the cytoplasm.
[4] After all substrates are bound, the conformational change from the open-pore state to the inward facing state is driven by the energetics of the favorable transport of Na+ ions.
[4] The (Figure 4b) allows release of one bile salt and two Na+ ions into the cytoplasm. In this conformation, the pore closes off relative to the extracellular side and opens to the cytoplasmic side.
[2] Afterwards, the remaining bile salt bound to NTCP shifts to the position the previous bile salt occupied, and the process repeats itself.
[4] The inherent amiphipathicity of bile acids allows passage through NTCP’s amphipathic pore (Figure 5)
Figure 5. Amphipathic pore of NTCP highlighting hydrophobic residues (red) and hydrophilic residues (white). (PDB:
7PQQ)
Mechanism of HBV/HDV Infection
After binding to NTCP in the , the viruses remain bound until low bile salt levels in the blood shift equilibria enough that endocytosis of the virus occurs. Once inside the cell, the viral genetic information is released.
The exact mechanism of how HBV and HDV bind to NTCP is not certain, on NTCP for HBV/HDV binding have been identified: residues and . An additional single-nucleotide polymorphism was discovered in East Asia involving being mutated from serine to phenylalanine. This mutation prevented HBV/HDV infection presumably by blocking the binding site in the pore of NTCP. Another mutation, replacing with tryptophan residues prevents HBV/HDV infection. Further zooming in on , it is probable that this mutation blocks the preS1 binding site of HBV/HDV. Myristoylation of the HBV/HDV capsid is also vital for recognition by NTCP, as well as residues 8-17 on HBV/HDV (sequence: NPLGFFPDHQ)[3]. Two mechanisms have been proposed for how HBV/HDV binds to NTCP. The first mechanism involves binding of the myristoyl group to the host cell membrane, while residues 8-17 interact with NTCP residues . The second mechanism involves binding of the myristoyl group with residues 157-165 in the pore.[6] After successful binding via one of these two proposed mechanisms, the virus is eventually endocytosed as described above.
Medical Relevance
Bile salts are derived from cholesterol, and they serve an important role in the mechanical digestion of fats and ultimately facilitate the chemical digestion of lipids.[7] Their amphipathicity allows them to solubilize hydrophobic fats for transport in aqueous bodily fluids.[7] Without bile salts, fats would spontaneously separate out of the aqueous solution in the duodenum and would not be accessible to pancreatic lipase for breakdown. Proper fat digestion requires both pancreatic lipase and bile; thus, NTCP's function in recycling bile salts is critical.[7] Additionally, bile acids play a major role in the regulation of lipid and energy metabolism. In mice, targeting NTCP-mediated bile acid was shown to treat obesity and obesity-related hepatosteatosis through the simultaneous dampening of intestinal fat absorption and increasing energy expenditure.[8]
Insight into NTCP's structure and function has implications for therapeutic treatment of HBV/HDV infection. The overlap in NTCP binding sites for bile salts and HBV/HDV viruses presents therapeutic issues in blocking HBV/HDV infection without inhibiting normal bile acid uptake. For example, mycludex B is a current first-class inhibitor of HDV infection, but suffers the drawback of hindering bile acid uptake. Potentially overcoming this, the inhibitory effect of antibody Nb87 on myr-preS1 binding shows potential for therapeutics that stabilize NTCP inward facing state as an allosteric inhibitor of viral cell entry. [6] With Nb87 bound, HBV/HDV infection was reduced, although transport of bile salts persisted. Another study has identified a ciclosporin derivative that has the capability to prevent HBV binding while still allowing NTCP to transport bile salts. [9] This small molecule is the first to successfully prevent infection against multiple HBV genotypes without hindering normal NTCP activity, highlighting the fact that anti-HBV activity can remain separate from NTCP function.[9] Future studies will work to identify more effective and safe ways to prevent infection without hindering normal bile acid uptake.