This is a default text for your page Harrison L. Smith/Sandbox1. Click above on edit this page to modify. Be careful with the < and > signs.
You may include any references to papers as in: the use of JSmol in Proteopedia [1] or to the article describing Jmol [2] to the rescue.
Introduction
The insulin receptor is a transmembrane protein receptor that is a vital proponent of cellular function. It plays a key role in a variety of cellular pathways including glucose homeostasis, regulation of lipid, protein, and carbohydrate metabolism, gene expression, and even modulation of brain neurotransmitter levels. This page focuses specifically on the insulin receptor's role in glucose homeostasis.
Structural Highlights
The insulin receptor is a dimer of heterodimers made of two alpha subunits and two beta subunits [3].The are on the extracellular side of the membrane and is critical for binding insulin. The that have the potential to interact with insulin on the extracellular side of the membrane, but it is generally more common for only one or two insulin molecules to bind to the receptor due to the occurrence of negative affinity at the binding site. The are transmembrane subunits that contain a tyrosine kinase region. Beta chains experience a conformation change that brings them from a V shape to a T shape upon activation or binding of an insulin molecule. When the two subunits are brought near to each other in the activated T form, each Tyrosine Kinase region is able to autophosphorylate its counterparts at particular Tyrosine locations. This aspect of the molecule has not yet been imaged.
Function

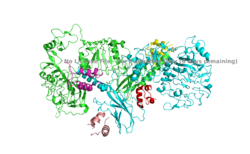
Figure 1. An image of the inactive Insulin Receptor Alpha subunit in the inverted V conformation. This image shows only a protomer of the alpha subunit because the entire alpha subunit dimer has been unable to be photographed because the transition state has yet to be determined.
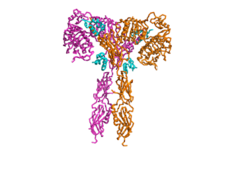
Figure 3. An image of the Insulin Receptor in T conformation (showing both Alpha and Beta subunits).
The insulin receptor's function in regards to glucose homeostasis is to begin the signaling pathway that will eventually move glucose transporters to the cell surface which will allow glucose to passively defuse into the cell. The glucose receptor is inactive in the absence of insulin. When insulin does bind to the receptor, it undergoes a conformation change, activating it. Once activated, the intracellular Beta subunits autophosphorylate, and downstream signaling begins by the phosphorylation of the Insulin Receptor Substrate (IRS).
Conformation Change
The insulin receptor has two conformations, an active and inactive state. The inactive form predominates in low-levels of circulating insulin, whereas the active conformation is seen when insulin binds to any of the 4 receptor sites. The inactive conformation resembles an inverted V (Figure 1), and the active conformation resembles a T (Figure 2). Upon the binding of insulin to any of the four binding sites, the conformation change will begin, causing the Beta subunit's tyrosine kinase domains to move close together, allowing them to autophosphorylate. This autophosphorylation is what activates the insulin receptor and allows it to participate in further downstream signaling pathways. [4].
Relevance
As mentioned in the Introduction, the insulin receptor is relevant to numerous biological functions of the body. In a healthy, normal-functioning human, each cell has many insulin receptors that reacts to insulin when blood glucose levels rise. Without properly functioning insulin receptors, medical intervention is necessary for survival.
Disease
One of the most common diseases involving the insulin receptor is diabetes mellitus. There are two types of diabetes- which are referred to as type 1 and type 2 diabetes. Type 1 diabetes is classified as "insulin dependent" and is characterized by an inability for the body to produce insulin. This is most often the result of damage or insufficiency in the Islets of Langerhans in the pancreas. Type 2 diabetes is classified as "insulin independent" and is the result of the body producing insufficient amounts of insulin, or not responding to the insulin. This often occurs because of high blood-glucose levels. Both types of diabetes are often treated with insulin injections, and diet and lifestyle changes. [5] [6].
Treatment of Diabetes with Insulin