Sandbox Reserved 994
From Proteopedia
| This Sandbox is Reserved from 20/01/2015, through 30/04/2016 for use in the course "CHM 463" taught by Mary Karpen at the Grand Valley State University. This reservation includes Sandbox Reserved 987 through Sandbox Reserved 996. |
To get started:
More help: Help:Editing |
Contents |
OXA-24 β-lactamase
|
Background
OXA-24 is a member of the carbapenem-hydrolyzing class D β-lactamases (CHDLs) and is expressed as a resistance mechanism by the bacteria Acinetobacter baumannii. In 1997, this resistant bacteria was involved in a nosocomial outbreak in a hospital in Spain.[1] Class D β-lactamases are clinically dangerous because they hydrolyze β-lactam antibiotics such as penicillins, cephalosporins, and carbapenems. Class D β-lactamases are classified as OXAs, which is in reference to their class designation as oxacillinases, however the terminology is somewhat misleading. While they do have a strong affinity for the antibiotic oxacillin[2], the OXAs have expanded to include penillinase, cephalosporinase, and carbapenemase activity in their spectrum. Due to their original designation as oxacillinases, however, the assignment of the prefix OXA has continued to be standard designation.
Structure
OXA-24 is a monomeric protein with an active site composed of a short α-helix and a β-sheet. The active site of OXA-24 is characterized by a (shown in pink on the structure) which is representative of Class D β-lactamases as a whole. The active site also contains a hydrophobic which contributes to the substrate specificity for carbapenems and is composed of an arrangement of the Tyr-112 and Met-223 side chains.[3] These residues block the active site and only allow a very specific binding configuration of antibiotics. The active site is overall positively charged and contains a sulfate ion along with other solvent molecules when no substrate is bound. The mechanism of attack is through the use of three : Serine-81, Carboxylated Lysine-84, and Serine-128. The hydroxyl chain of Ser-128 conforms in the direction of the active-serine Ser-81, and contributes to the catalytic mechanism.[3]
Bacterial Resistance
Since the discovery of penicillin by Alexander Flemming in 1928, antibiotics have revolutionized the medical world. Penicillin is known as a β-lactam antibiotic, which is characterized by a four-membered β-lactam ring (a cyclic amide). There are four classes of β-lactam antibiotics: monobactams, which are the simplest class of β-lactam and aren’t fused to any rings, penicillins, which have a thiazole ring fused to the β-lactam, cephalosporins, which contain a thiazine ring, and lastly carbapenems, which are fused with a pyrrole ring and are considered a last line of defense. [4] β-lactam antibiotics are the most widely used class of antibiotics because they successfully fight most bacterial infections by inhibiting cell wall synthesis. Their mechanism of action is through inhibition of the transpeptidase enzymes, which are located in the bacterial cell membrane. Transpeptidase is alternatively referred to as a penicillin-binding protein (PBP) and is responsible for catalyzing the cross-linking of the bacterial cell wall [5]. Bacteria have cell walls which are largely made of a material called peptidoglycan, composed of N-Acetylmuramic acid (NAM) and N-Acetylglucosamine (NAG), which the cell uses to protect against lysis from changing osmotic pressure. β-lactams are a group of antibiotics that block the NAM cross linking in the bacterial cell wall by mimicing the structure of the terminal D-alanine chain of peptidoglycan and irreversibly binding to the enzymes that cross-link NAM subunits (PBP).[6]-lactams and irreversibly bind to PBP, disrupting the cross-linking process that is critical to cell wall synthesis. As a result, the bacterial cell wall is compromised and the bacteria lyse and die.[7]
Due to overperscription and misuse of antibiotics, bacteria have been able to develop resistance mechanisms. One of these resistance mechanisms is through the expression of β-lactamases, which have evolved as a seperate enzyme over millions of years from PBP.[8] β-lactamases act by hydrolyzing the β-lactam ring, which renders the antibiotic inactive before it has a chance to inhibit the transpeptidase enzymes.[9] β-lactamases are grouped into four different classes (A, B, C and D); all of which, with the exception of class B, use a serine based mechanism for destruction of β-lactams. Class B β-lactamases use zinc ions for hydrolysis. Class D was distinguished from other serine β-lactamases in the late 1980s, due to having an affinity for oxacillin as its substrate in addition to other antibiotics.[10] Even more concerning is that the class D β-lactamases, or OXAs, are not inhibited by current clinical β-lactamase inhibitors such as clavulanic acid. OXA-24, which has considerable carbapenemase activity, poses a dangerous clinical threat due to the absence of an effective inhibitor.
β-lactam Hydrolysis
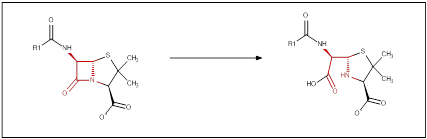
Catalytic Activity
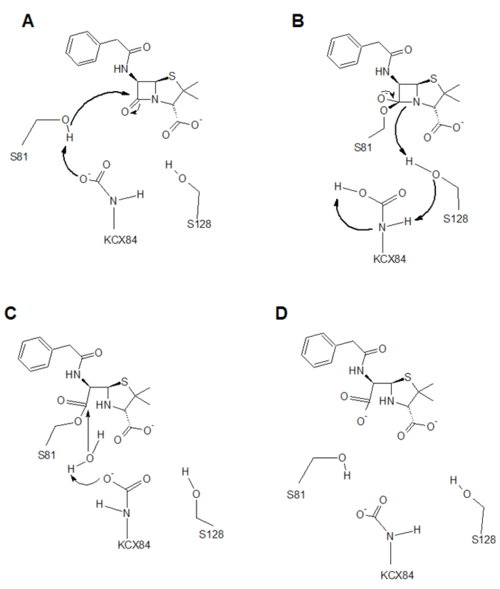
There are three catalytic residues involved in the hydrolysis of β-lactam antibiotics. Serine-81 is the catalytic serine, which performs a nucleophilic attack on the β-lactam ring after being deprotonated by the carboxylated lysine-84 (KCX84). This carboxylated lysine is formed by carbon dioxide in the environment engaging in unfavorable interactions with the hydrophobic pocket of OXA-24, so it carboxylates Lysine-84 (A).[2]
The second step (B) forms a high energy intermediate. The cyclic amide from the β-lactam deprotonates Serine-128 (S128), which proceeds to deprotonate the amine on KCX84, which deprotonates the carboxylate group. This high energy intermediate resolves to form the stable acyl-enzyme intermediate.[2]
The third step (C) proceeds with the use of a catalytic water, which is deprotonated by KCX84. The water now can mount a nucleophilic attack on the ester linkage connecting S81 and the hydrolyzed β-lactam. This forms a high energy dissociation intermediate, where S81 is released by a mechanism, which has not quite yet been determined. It is suspected that it deprotonates KCX84, but this has not yet been confirmed.[2]
In step four (D), the enzyme is successfully regenerated and the hydrolyzed β-lactam antibiotic is released back into solution. OXA-24 is now free to hydrolyze another substrate and the antibiotic has been rendered useless.[2]
References
- ↑ Bou, German, Antonio Oliver, and Jesus Martinez-Beltran. "OXA-24, a Novel Class D β-Lactamase with Carbapenemase Activity in an Acinetobacter Baumannii Clinical Strain." Antimicrobial Agents and Chemotherapy 44, no. 6 (2000): 1556-561. Accessed February 19, 2015. http://aac.asm.org/content/44/6/1556.full
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Leonard DA, Bonomo RA, Powers RA. Class D beta-lactamases: a reappraisal after five decades. Acc Chem Res. 2013 Nov 19;46(11):2407-15. doi: 10.1021/ar300327a. Epub 2013 Jul, 31. PMID:23902256 doi:http://dx.doi.org/10.1021/ar300327a
- ↑ 3.0 3.1 Santillana, Elena et al. “Crystal Structure of the Carbapenemase OXA-24 Reveals Insights into the Mechanism of Carbapenem Hydrolysis.” Proceedings of the National Academy of Sciences of the United States of America 104.13 (2007): 5354–5359. PMC. Web. 25 Mar. 2015.
- ↑ Konaklieva, Monika. "Molecular Targets of β-Lactam-Based Antimicrobials: Beyond the Usual Suspects." Antibiotics 2014, 3(2), 128-142; doi:10.3390/antibiotics3020128
- ↑ Bush, K, G A Jacoby, and A A Medeiros. “A Functional Classification Scheme for Beta-Lactamases and Its Correlation with Molecular Structure.” Antimicrobial Agents and Chemotherapy 39.6 (1995): 1211–1233. Print.
- ↑ Bauman, Robert W. "Controlling Microbial Growth in the Body: Antimicrobial Drugs." In Microbiology with Diseases by Taxonomy, 287-299. 4th ed. Glenetview, IL: Pearson, 2014.
- ↑ Patrick, G. (2005). Antibacterial Agents. An Introduction to Medicinal Chemistry (3rd Ed), pages 388-414.
- ↑ Meroueh, S.O; Minasov, G; Lee, W; Shoichet, B.K; Mobashery, S. Structural aspects for evolution of beta-lactamases from penicillin-binding proteins. J. Am. Chem Soc. (2003), 125, 9612-9618.
- ↑ Neu, Harold. "The Crisis in Antibiotic Resistance." Science (1992) 257, 5073. ProQuest Medical Library: p. 1064-1072.
- ↑ Bush K, Jacoby GA. Updated functional classification of beta-lactamases. Antimicrob Agents Chemother. 2010 Mar;54(3):969-76. doi: 10.1128/AAC.01009-09., Epub 2009 Dec 7. PMID:19995920 doi:http://dx.doi.org/10.1128/AAC.01009-09
