Introduction
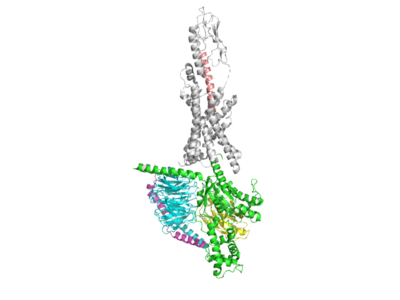
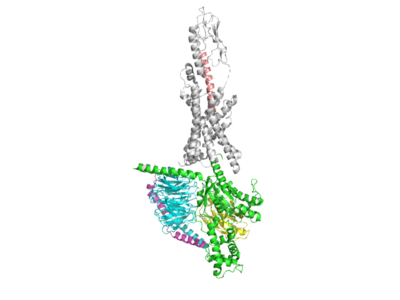
Figure 1: GLPR from pymol
History
The discovery, clinical development, and characterization of glucagon-like-peptide-1 (GLP-1) encompasses more than 30 years of research from many different scientists/investigators. GLP-1 alongside gastric inhibitory peptide (GIP) are the two primary incretin hormones released by pancreatic beta cells of the intestines following the ingestion of glucose.
Function
GLP-1 plays various critical roles in biological processes throughout the body. In adipose tissues, GLP-1 facilitates fat deposition. In bone, GLP-1 inhibits bone absorption. In the brain, both GLP-1 and GIP are involved in memory formation as well as the control of appetite.
Within the pancreas, GLP-1 promotes beta cell proliferation and inhibit apoptosis, allowing for clinically-desirable insulinotropic effects.
GLP-1 exerts its effects by binding to the GLP-1 receptor (GLP-1R) which stimulate effects in the body via G-protein coupled signaling. Receptor binding activates and increases the level of intracellular cyclic monophosphate (cAMP) in pancreatic beta cells as well as glucose-dependent insulin secretion.
Relevance
Marketed GLP-1R agonists such as dulaglutide, exenatide, liraglutide, and semaglutide represent an expanding drug class with beneficial therapeutic effects for those suffering from type II diabetes and obesity. In more recent years, co-agonist drugs which stimulate both the GLP-1R and GIPR pathways have been synthesized. These co-agonist drugs provide serious promise with regards to assisting those affected by the aforementioned conditions. The co-agonist drug, Tirzepatide, is regarded as one of the most promising candidates for better treatment of obesity and type II diabetes by improving weight reduction and glycemic control.
In this review page, we present the signaling pathways as well as structural highlights within the GLP-1 GPCR pathway in the pancreatic beta cell, focusing on its relevance with regards to the therapeutic effects of the Tirzepatide drug.
Structure
Extracellular Domain
Broadly the extracellular reactions between GLP-1 and GLP-1R lie between residues 15-32 on the peptide GLP-1. Residues L32, F28, W31 of the peptide and L36 and W214 of the receptor all utilize hydrophobic interactions or van der waals for affinity and binding, but exclusively F28, W31, and W214 have pi stacking which future maximizes interactions to increase binding. Furthermore, there is a strong hydrogen bond between D15 of the peptide to the R380 receptor. Van der Waals interactions continue on the residues Y19, L20, and V16 on the peptide as they interact with L141 and L210 of the receptor. Another hydrogen bond between E27 and Q21 also occurs. Finally, there is a patch of extensive hydrogen bonding in an almost chainlike fashion goin from L32 of the receptor to E21 of the peptide, to R299 of the receptor, to the S17 of the peptide which then interacts with Y205 and T298 both of the receptor.
Active Site/Binding Site
The transmembrane core is key to the active site/binding site. One of the main interactions between GLP-1 and GLP-1R includes the hydrogen bond between H7 and Q234 as the N-terminus of the peptide is bound to the transmembrane domain of the receptor. This interaction provides the most stability within the structure. It is further enhanced by hydrophobic interactions between residues V16 and F12 of the peptide and L384 and L141 of the receptor . Notably there is a hydrogen bond T13 of the peptide and K197 of the receptor. There is also a stabilizing hydrogen bond between S17 and E21 of GLP to R299 of the GLP-1R which anchors the GLP-1 peptide to the binding site of the receptor .
Intracellular Domain
The Intracellular domain of GLP-1 contains the C-terminus domain. Once the GLP-1 ligand stimulates the active site, then conformational changes occur within the intracellular regions. The intracellular domain of the GLP-1 ligand interacts with various intracellular proteins and signaling molecules, initiating a series of events that regulate insulin secretion, inhibit glucagon secretion, slow gastric emptying, and promote satiety, among other effects.
Applications
Tirzepatide
The co-agonist drug, Tirzepatide, is regarded as one of the most promising candidates for better treatment of obesity and type II diabetes by improving weight reduction and glycemic control. Here is a general overview of the Tirzepatide pepetide bound to the GLP-1R . Tirzepatide is a dual agonist of the glucagon-like-peptide-1 receptor (GLP-1R) and the glucose-dependent insulinotropic polypeptide receptor (GIPR). Co-agonism of both GLP-1 and GIP pathways provides beneficial therapeutic effects by mimicking desirable components of each respective pathway. Tirzepatide exhibits similar pharmacology to the native GIP pathway, but differs with regards to the GLP-1 pathway, as it shows biased signaling of cAMP. This biased signaling, also called differential signaling, allows for the co-agonist drug to increase efficacy in glucose control and body weight regulation for treating type II diabetes as well as obesity.
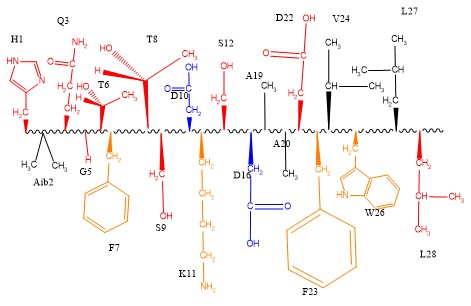
One way in which the Tirzepatide peptide fosters biased signaling is by utilizing particular residues from both GLP-1 and GIP in order to carefully stimulate parts of both pathways.
 Figure 1. The tirzepatide ligand can be viewed as a combination of both GLP-1 and GIP natural hormones. Shown in red are all the modified residues of tirzepatide. The blue residues are residues that both Tirzepatide and GLP-1 share.
Figure 1. The tirzepatide ligand can be viewed as a combination of both GLP-1 and GIP natural hormones. Shown in red are all the modified residues of tirzepatide. The blue residues are residues that both Tirzepatide and GLP-1 share.
One way in which the Tirzepatide peptide differs from both GLP-1 and GIP is seen through two mutations at residue sites 2 and 13. These residues have been mutated to mutant AIB residue which is physiologically vital for the performance of the drug as it prevents cleavage from the enzyme DPP-4, which normally cleaves the native GLP-1 peptide . Tirzepatide binds similarly to the native GLP-1 peptide to its GLP-1R by forming hydrogen bonds with the receptor. Y1 of the Tirzepatide peptide is seen hydrogen bonding with Q234 of the GLP-1R, allowing for the peptide to be anchored to the receptor . The Tirzepatide drug is furthermore stabilized to the GLP-1R through pi-stacking interactions between Y10 of the drug and Y145 of the receptor .
Additionally, there are certain aspects of the Tirzepatide peptide design which favor the GIP pathway over the GLP-1 pathway. This area of biased signalling is seen through steric clashing between the Tirzepatide peptide and the GLP-1R, which was not seen with the native GLP-1 bound to GLP-1R
. The lack of steric clashing in the native interaction suggests that this area of the Tirzepatide peptide is important for biased GIP pathway stimulation as an interaction which was found to increase stability of the native GLP-1 bound to GLP-1R is lost with regards to the co-agonist drug Tirzepatide.
Implications
Tirzepatide's dual action on both the GIP and GLP-1 pathways offers the potential for superior glycemic control and weight loss compared to existing therapies. Individuals with type two diabetes or obesity can benefit from Tirzepatide, taking a subcutaneous injection weekly instead of needing to closely monitor a restrictive diet.
Future Directions
The future direction of Tirzapetide and its pharmaceutical uses include further testing of its effects both short term and long term. Current adverse side effects need to be continually monitored, as do all pharmaceuticals. Tirzepatide’s dual action on both GIP and GLP-1 receptors create a greater effect of glucose control and body weight regulation than the body’s natural ligands, however work can continue to be done on a triple-acting agonist. A possible drug technology that is currently in development at Eli Lilly not only effects the GIP and GLP-1 protein receptors, but also glucagon receptors. The drug is known as 'Peptide 20'.This promises to be a revolutionary drug for type 2 diabetes and weight loss.
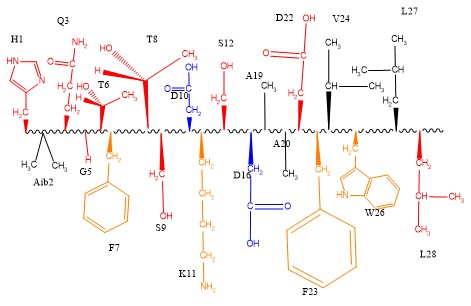
Figure 2. The structure of Peptide 20 will interact with the GLP-1 receptor in many different ways. Shown are several residues and their interactions. Red shows hydrogen bonding, black shows Van der Waals interactions, orange shows pi stacking, and blue shows salt bridges. NOTE: not all residues are shown.