Sandbox Reserved 1791
From Proteopedia
(Difference between revisions)
| (3 intermediate revisions not shown.) | |||
| Line 4: | Line 4: | ||
== Introduction == | == Introduction == | ||
| - | [[Image:TSH system1.png|300 px|right|thumb| Figure 1: An overview of the Thyroid System. A depiction of signaling cascade from the hypothalamus ending in the release of TSH causing T3 and T4 production and its effects. The mechanism of regulation is also shown by negative feedback from the T3 and T4 hormones. Source: [https://commons.wikimedia.org/wiki/File:Figure_37_04_01.png]]] | + | [[Image:TSH system1.png|300 px|right|thumb| Figure 1: An overview of the Thyroid System. A depiction of signaling cascade from the hypothalamus ending in the release of TSH causing T3 and T4 production and its effects. The mechanism of regulation is also shown by [https://biologydictionary.net/negative-feedback/ negative feedback] from the T3 and T4 hormones. Source: [https://commons.wikimedia.org/wiki/File:Figure_37_04_01.png]]] |
| - | '''Thyroid Stimulating Hormone Receptor (TSHR)''' is a [https://proteopedia.org/wiki/index.php/GPCRs G-Protein Coupled Receptor (GPCR)] found in human thyroid follicles<ref name="Faust"> DOI 10.1038/s41586-022-05159-1</ref>. TSHR is activated by the [https://en.wikipedia.org/wiki/Thyroid-stimulating_hormone Thyroid Stimulating Hormone (TSH)] also known as thyrotropin. Activation of TSHR initiates a signaling pathway for the production of thyroid hormones such as [https://en.wikipedia.org/wiki/Triiodothyronine T<sub>3</sub>] and [https://en.wikipedia.org/wiki/Thyroid_hormones T<sub>4</sub>] | + | '''Thyroid Stimulating Hormone Receptor (TSHR)''' is a [https://proteopedia.org/wiki/index.php/GPCRs G-Protein Coupled Receptor (GPCR)] found in human thyroid follicles<ref name="Faust"> DOI 10.1038/s41586-022-05159-1</ref>. TSHR is activated by the [https://en.wikipedia.org/wiki/Thyroid-stimulating_hormone Thyroid Stimulating Hormone (TSH)] also known as thyrotropin. Activation of TSHR initiates a signaling pathway for the production of thyroid hormones such as [https://en.wikipedia.org/wiki/Triiodothyronine T<sub>3</sub>] and [https://en.wikipedia.org/wiki/Thyroid_hormones T<sub>4</sub>] that are used to regulate the metabolism(Fig 1). |
== Structure== | == Structure== | ||
TSHR forms an active signaling complex with TSH and G<sub>s</sub> proteins. This is called the <scene name=scene name='95/952720/Tsh-tshr-gs_complex/3'>TSH-TSHR-Gs Complex</scene>. TSH contains an α and a β subunit. The α subunit is a shared subunit amongst glycoproteins. The β subunit is unique to TSH. TSH binds to the extracellular domain of TSHR <ref name="Duan"> DOI 10.1038/s41586-022-05173-3</ref>. | TSHR forms an active signaling complex with TSH and G<sub>s</sub> proteins. This is called the <scene name=scene name='95/952720/Tsh-tshr-gs_complex/3'>TSH-TSHR-Gs Complex</scene>. TSH contains an α and a β subunit. The α subunit is a shared subunit amongst glycoproteins. The β subunit is unique to TSH. TSH binds to the extracellular domain of TSHR <ref name="Duan"> DOI 10.1038/s41586-022-05173-3</ref>. | ||
| Line 23: | Line 23: | ||
== Active vs. Inactive State == | == Active vs. Inactive State == | ||
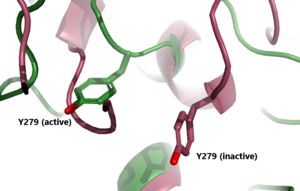
| - | In its resting state without TSH bound, TSHR is in the <scene name='95/952720/Inactivetshr/8'>inactive state</scene>, also known as the "down" state because the LRRD is pointing down. When TSH binds to TSHR, steric clashes between TSH and the cell-membrane cause TSHR to take on the <scene name='95/952720/Inactivetshr/6'>active or "up" state</scene> ( | + | In its resting state without TSH bound, TSHR is in the <scene name='95/952720/Inactivetshr/8'>inactive state</scene>, also known as the "down" state because the LRRD is pointing down. When TSH binds to TSHR, steric clashes between TSH and the cell-membrane cause TSHR to take on the <scene name='95/952720/Inactivetshr/6'>active or "up" state</scene> (Fig 2). During this transition, the LRRD rotate 55° along an axis perpendicular to the cell membrane. This rotation is initiated by conformational changes within the <scene name='95/952719/Hinge_region_spin/3'>Higne Region</scene>, specifically at the <scene name='95/952720/Hinge_region_residues/3'>Tyr279 residue</scene>, located in the Hinge Region. Y279 moves 6 Å relative to I486, which is a residue located in the Transmembrane Region nearby Y279<ref name="Faust"/> (Fig 3). |
The active form is favored when <scene name='95/952719/Active_form/6'>TSHR is bound to TSH</scene>. The structure can be seen as straight. The same straight conformation is observed when TSHR is bound with M22. The inactive form is found when <scene name='95/952719/Inactive_form/7'>TSHR is bound with K1</scene> of TSHR is found when bound with K1. The overall structure of the molecule is bent when K1 is bound. | The active form is favored when <scene name='95/952719/Active_form/6'>TSHR is bound to TSH</scene>. The structure can be seen as straight. The same straight conformation is observed when TSHR is bound with M22. The inactive form is found when <scene name='95/952719/Inactive_form/7'>TSHR is bound with K1</scene> of TSHR is found when bound with K1. The overall structure of the molecule is bent when K1 is bound. | ||
| Line 40: | Line 40: | ||
[https://www.mayoclinic.org/diseases-conditions/hyperthyroidism/symptoms-causes/syc-20373659 Hyperthyroidism] is when the thyroid is overactive which leads to upregulation of the metabolism. This overactive state can be initiated by antibodies like M22. M22 antibody maintains TSHR in the active conformation. In this conformation, the thyroid continues to make T3 and T4, overstimulating the metabolism. Symptoms of hyperthyroidism include fast or irregular heartbeats, tiredness, increased hunger, sleep problems, enlarged thyroid gland, and sensitivity to heat. [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease Grave's Disease] is the most common cause of hyperthyroidism. This is an autoimmune disorder that causes your body to attack the thyroid gland<ref name="Luca">Chiovato L, Magri F, Carlé A. Hypothyroidism in Context: Where We've Been and Where We're Going. Adv Ther. 2019 Sep;36(Suppl 2):47-58. doi: 10.1007/s12325-019-01080-8. Epub 2019 Sep 4. PMID: 31485975; PMCID: PMC6822815. [DOI: 10.1007/s12325-019-01080-8 https://pubmed.ncbi.nlm.nih.gov/31485975/]</ref>. When someone has Hypothyroidism the body produces M22 that leads to overactive metabolism functions. | [https://www.mayoclinic.org/diseases-conditions/hyperthyroidism/symptoms-causes/syc-20373659 Hyperthyroidism] is when the thyroid is overactive which leads to upregulation of the metabolism. This overactive state can be initiated by antibodies like M22. M22 antibody maintains TSHR in the active conformation. In this conformation, the thyroid continues to make T3 and T4, overstimulating the metabolism. Symptoms of hyperthyroidism include fast or irregular heartbeats, tiredness, increased hunger, sleep problems, enlarged thyroid gland, and sensitivity to heat. [https://www.niddk.nih.gov/health-information/endocrine-diseases/graves-disease Grave's Disease] is the most common cause of hyperthyroidism. This is an autoimmune disorder that causes your body to attack the thyroid gland<ref name="Luca">Chiovato L, Magri F, Carlé A. Hypothyroidism in Context: Where We've Been and Where We're Going. Adv Ther. 2019 Sep;36(Suppl 2):47-58. doi: 10.1007/s12325-019-01080-8. Epub 2019 Sep 4. PMID: 31485975; PMCID: PMC6822815. [DOI: 10.1007/s12325-019-01080-8 https://pubmed.ncbi.nlm.nih.gov/31485975/]</ref>. When someone has Hypothyroidism the body produces M22 that leads to overactive metabolism functions. | ||
=== Hypothyroidism === | === Hypothyroidism === | ||
| - | [https://www.mayoclinic.org/diseases-conditions/hypothyroidism/symptoms-causes/syc-20350284#:~:text=Hypothyroidism%20happens%20when%20the%20thyroid,symptoms%20in%20its%20early%20stages Hypothyroidism] is when the thyroid is underactive leading to a decrease in metabolism function. K1 antibody binds to TSHR to promote the inactive confirmation that is conserved despite the presence of TSH. This does not allow for the signaling of the T3 and T4 hormones to upregulate the metabolism. The symptoms of this include slow or irregular heartbeats, tiredness, muscle aches, memory problems, jaundice, and sensitivity to cold. [https://www.mayoclinic.org/diseases-conditions/hashimotos-disease/symptoms-causes/syc-20351855 Hasimoto's disease] is an example of hypothyroidism. This is an autoimmune disorder that causes your body to attack the healthy cells of the thyroid. Specifically causing the death of the cells that produce the thyroid hormones. When the thyroid fails to produce its hormones it activates TSH production through a negative feedback mechanism<ref name="Luca">. When someone has Hashimoto's disease the body produces the K1 antibody it does not respond to the negative feedback system and the body cannot regulate the metabolism. | + | [https://www.mayoclinic.org/diseases-conditions/hypothyroidism/symptoms-causes/syc-20350284#:~:text=Hypothyroidism%20happens%20when%20the%20thyroid,symptoms%20in%20its%20early%20stages Hypothyroidism] is when the thyroid is underactive leading to a decrease in metabolism function. K1 antibody binds to TSHR to promote the inactive confirmation that is conserved despite the presence of TSH. This does not allow for the signaling of the T3 and T4 hormones to upregulate the metabolism. The symptoms of this include slow or irregular heartbeats, tiredness, muscle aches, memory problems, [https://my.clevelandclinic.org/health/diseases/15367-adult-jaundice jaundice], and sensitivity to cold. [https://www.mayoclinic.org/diseases-conditions/hashimotos-disease/symptoms-causes/syc-20351855 Hasimoto's disease] is an example of hypothyroidism. This is an autoimmune disorder that causes your body to attack the healthy cells of the thyroid. Specifically causing the death of the cells that produce the thyroid hormones. When the thyroid fails to produce its hormones it activates TSH production through a [https://biologydictionary.net/negative-feedback/ negative feedback mechanism]<ref name="Luca">. When someone has Hashimoto's disease the body produces the K1 antibody it does not respond to the negative feedback system and the body cannot regulate the metabolism. |
== Student Contributions == | == Student Contributions == | ||
*Alex Kem | *Alex Kem | ||
Current revision
| This Sandbox is Reserved from February 27 through August 31, 2023 for use in the course CH462 Biochemistry II taught by R. Jeremy Johnson at the Butler University, Indianapolis, USA. This reservation includes Sandbox Reserved 1765 through Sandbox Reserved 1795. |
To get started:
More help: Help:Editing |
Thyroid Stimulating Hormone Receptor (TSHR)
| |||||||||||
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Faust B, Billesbolle CB, Suomivuori CM, Singh I, Zhang K, Hoppe N, Pinto AFM, Diedrich JK, Muftuoglu Y, Szkudlinski MW, Saghatelian A, Dror RO, Cheng Y, Manglik A. Autoantibody mimicry of hormone action at the thyrotropin receptor. Nature. 2022 Aug 8. pii: 10.1038/s41586-022-05159-1. doi:, 10.1038/s41586-022-05159-1. PMID:35940205 doi:http://dx.doi.org/10.1038/s41586-022-05159-1
- ↑ 2.0 2.1 2.2 2.3 Duan J, Xu P, Luan X, Ji Y, He X, Song N, Yuan Q, Jin Y, Cheng X, Jiang H, Zheng J, Zhang S, Jiang Y, Xu HE. Hormone- and antibody-mediated activation of the thyrotropin receptor. Nature. 2022 Aug 8. pii: 10.1038/s41586-022-05173-3. doi:, 10.1038/s41586-022-05173-3. PMID:35940204 doi:http://dx.doi.org/10.1038/s41586-022-05173-3
- ↑ 3.0 3.1 Fokina, E.F., Shpakov, A.O. Thyroid-Stimulating Hormone Receptor: the Role in the Development of Thyroid Pathology and Its Correction. J Evol Biochem Phys 58, 1439–1454 (2022). [DOI:10.1134/S0022093022050143 https://doi.org/10.1134/S0022093022050143]
- ↑ Chen CR, McLachlan SM, Rapoport B. Thyrotropin (TSH) receptor residue E251 in the extracellular leucine-rich repeat domain is critical for linking TSH binding to receptor activation. Endocrinology. 2010 Apr;151(4):1940-7. doi: 10.1210/en.2009-1430. Epub 2010 Feb 24. PMID: 20181794; PMCID: PMC2851189. [DOI 10.1210/en.2009-1430 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2851189/]
- ↑ 5.0 5.1 Goel R, Raju R, Maharudraiah J, Sameer Kumar GS, Ghosh K, Kumar A, Lakshmi TP, Sharma J, Sharma R, Balakrishnan L, Pan A, Kandasamy K, Christopher R, Krishna V, Mohan SS, Harsha HC, Mathur PP, Pandey A, Keshava Prasad TS. A Signaling Network of Thyroid-Stimulating Hormone. J Proteomics Bioinform. 2011 Oct 29;4:10.4172/jpb.1000195. PMID:24255551 doi:10.4172/jpb.1000195
- ↑ Maeda S, Koehl A, Matile H, Hu H, Hilger D, Schertler GFX, Manglik A, Skiniotis G, Dawson RJP, Kobilka BK. Development of an antibody fragment that stabilizes GPCR/G-protein complexes. Nat Commun. 2018 Sep 13;9(1):3712. doi: 10.1038/s41467-018-06002-w. PMID:30213947 doi:http://dx.doi.org/10.1038/s41467-018-06002-w
- ↑ 7.0 7.1 Nunez Miguel R, Sanders J, Chirgadze DY, Furmaniak J, Rees Smith B. Thyroid stimulating autoantibody M22 mimics TSH binding to the TSH receptor leucine rich domain: a comparative structural study of protein-protein interactions. J Mol Endocrinol. 2009 May;42(5):381-95. Epub 2009 Feb 16. PMID:19221175 doi:10.1677/JME-08-0152
- ↑ Furmaniak J, Sanders J, Sanders P, Li Y, Rees Smith B. TSH receptor specific monoclonal autoantibody K1-70TM targeting of the TSH receptor in subjects with Graves' disease and Graves' orbitopathy-Results from a phase I clinical trial. Clin Endocrinol (Oxf). 2022 Jun;96(6):878-887. doi: 10.1111/cen.14681. Epub 2022 Feb 6. PMID: 35088429; PMCID: PMC9305464. [DOI 10.1111/cen.14681]
- ↑ Smits G, Govaerts C, Nubourgh I, Pardo L, Vassart G, Costagliola S. Lysine 183 and glutamic acid 157 of the TSH receptor: two interacting residues with a key role in determining specificity toward TSH and human CG. Mol Endocrinol. 2002 Apr;16(4):722-35. doi: 10.1210/mend.16.4.0815. PMID: 11923469. [DOI: 10.1210/mend.16.4.0815 https://pubmed.ncbi.nlm.nih.gov/11923469/]
- ↑ 10.0 10.1 Chiovato L, Magri F, Carlé A. Hypothyroidism in Context: Where We've Been and Where We're Going. Adv Ther. 2019 Sep;36(Suppl 2):47-58. doi: 10.1007/s12325-019-01080-8. Epub 2019 Sep 4. PMID: 31485975; PMCID: PMC6822815. [DOI: 10.1007/s12325-019-01080-8 https://pubmed.ncbi.nlm.nih.gov/31485975/]
![Figure 1: An overview of the Thyroid System. A depiction of signaling cascade from the hypothalamus ending in the release of TSH causing T3 and T4 production and its effects. The mechanism of regulation is also shown by negative feedback from the T3 and T4 hormones. Source: [1]](/wiki/images/thumb/1/1d/TSH_system1.png/300px-TSH_system1.png)

![Figure 4: T3 and T4 role in TSH concentration: Highlighting the problem when under or overactive on the metabolism. When an antibody is bound to TSHR and cannot respond to the negative feedback look the metabolism experiences a shift outside of equilibrium resulting in a wide array of side effects. [2]](/wiki/images/thumb/5/5f/T3t4levels.jpeg/400px-T3t4levels.jpeg)
