Introduction
![Figure 1: An overview of the Thyroid System. A depiction of signaling cascade from the hypothalamus ending in the release of TSH causing T3 and T4 production and its effects. The mechanism of regulation is also shown by negative feedback from the T3 and T4 hormones. Source: [1]](/wiki/images/thumb/1/1d/TSH_system1.png/300px-TSH_system1.png)
Figure 1: An overview of the Thyroid System. A depiction of signaling cascade from the hypothalamus ending in the release of TSH causing T3 and T4 production and its effects. The mechanism of regulation is also shown by negative feedback from the T3 and T4 hormones. Source:
[1]Thyroid Stimulating Hormone Receptor (TSHR) is a G-Protein Coupled Receptor (GPCR) found in human thyroid follicles[1]. TSHR is activated by the Thyroid Stimulating Hormone (TSH) also known as thyrotropin. Activation of TSHR initiates a signaling pathway for the production of thyroid hormones such as T3 and T4 (Fig 1). These hormones are used to regulate the metabolism.
Structure
TSHR forms an active signaling complex with TSH and Gs proteins. This is called the . TSH contains an α and a β subunit. The α subunit is a shared subunit amongst glycoproteins. The β subunit is unique to TSH. TSH binds to the extracellular domain of TSHR [2].
: Leucine Rich Region Domain (coral), the hinge region (blue-purple), and the transmembrane region(rainbow). The leucine rich region domain is the extracellular TSH ligand domain. The hinge connects the Leucine Rich Repeat Domain and the Transmembrane Region. It provides flexibility for the switch between the active and inactive state of TSHR. The transmembrane region is located within the plasma membrane. Its function transmit the extracellular signal across the membrane to the intracellular G-proteins bound to the N-terminus of the transmembrane region[2]. Activated G-proteins then signal a robust intracellular signaling cascade.
Leucine Rich Domain
The is the extracellular ligand binding region of TSHR. Connects to the Hinge Region at its C-terminus. It is made up of polar residues in a concave parallel β-sheet composed of leucine-rich repeats where TSH binds and is called the [2]. The LRRD concave surface is where the TSH antibody antagonist, K1, binds as well as the agonist M22. Two specific LYS residues interact with the substrate to result in a structural change of the molecule. N-glycans attached to asparagine residues play a large role in the binding of TSH. Negative charge on these N glycans contributes to the polarity of the binding pocket which mediates the binding efficiency of TSH. Four of the five N glycan sites must be glycosylated for TSHR to be in the active form[3].
Hinge Region
The (purple-blue) connects the Transmembrane Region to the Leucine Rich Domain. Also referred to as the signaling specificity domain the hinge region plays a dual role in both TSH binding and signal transduction. [4]. The hinge region is made up of two α-helices connected via disulfide bonds. The disulfide bonds are important for transmitting the signal to the Transmembrane region. The two helices help orient TSH properly for LRRD binding. It is proposed that the Asp386, Tyr385, and Tyr387 create a negative-charged region on the Helix. This negatively charged region interacts with the positively charged region of TSH created by residue Arg54. These interactions are essential for TSH binding, however, they are not required for the activation of TSHR. This is known because the M22 antibody is able to activate TSHR even though it does not have an Arg54 residue Conformational changes in this hinge region, specifically the orientation of , which is located in the hinge region, are responsible for the bringing TSHR into the active state [1]
Transmembrane Region
() is embedded within the cell membrane, like other G-protein receptors, it is composed of a 7-pass helix [1]. The transmembrane region is surrounded by a "belt" of . When cholesterol binding sites are mutated, TSHR activity decreases. These cholesterols are likely important for TSHR function [2]. Additionally, at the N-terminus, the transmembrane region binds to the , which are located intracellularly [5]. The G-proteins are made up of three subunits: α, β, and γ. Nb35 a fourth subunit that stabilizes the structure by binding between the Gα and Gβ interface[6]. When TSHR is activated, it causes the Gα subunit to dissociate from the Gβγ subunits. The Gα subunit is responsible for activating adenylyl cyclase, phospholipase C, and ion channels. This sets off the robust intracellular signaling cascade[5].
Antibodies
Antibodies are an important part of the thyroid response. These proteins are made in an immune system response to get rid of unwanted antigens in the body. Thyroid antibodies are made when the body attacks the thyroid tissues. These antibodies are made to mimic TSH (Thyroid Stimulating Hormone). TSH is released from the pituitary gland to bind to TSHR and stimulate the thyroid to make T3 and T4 hormones to regulate the metabolism. These thyroid antibodies bind to the concave surface of the LRD.
M22
M22 is an activating antibody for TSHR. This antibody mimics TSH to activate the thyroid gland to produce T3 and T4 hormones. M22 makes a stronger interaction with TSHR than TSH does due to a larger number of hydrogen bonds and salt bridges. This interaction is key for understanding why M22 activates TSHR and does not release TSHR to go into the inactive state even when T3 and T4 levels are high[7].
K1
K1 is an inhibitory antibody. This antibody mimics [TSH and blocks it from binding. When K1 is bound it does not allow TSHR to be in the active state like TSH and M22 do to produce T3 and T4 hormones.
Active vs. Inactive State
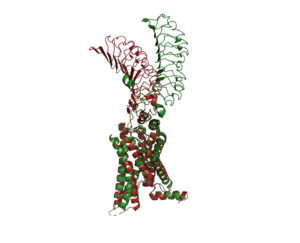
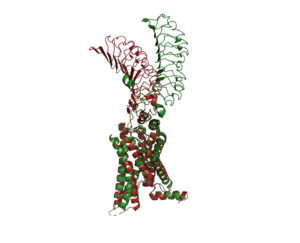
Figure 2: An overview of the Inactive (red) vs Active (green) state of TSHR. PDB: 7WX5
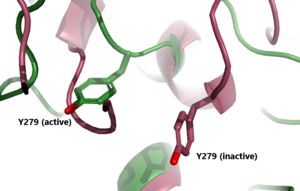
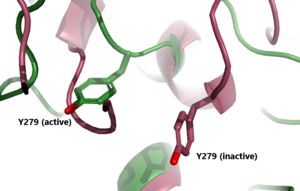
Figure 3: A zoomed in view of the Y279 residue in the Hinge Region of TSHR, showing the 6 angstrom move of Y279 during the activation of TSHR. Active TSHR is shown in green (PDB: 7t9i) and inactive TSHR is shown in pink (PDB: 7t9m).
In its resting state without TSH, TSHR is in the , also considered the "down" state because the LRRD is pointing down. When TSH binds to TSHR, steric clashes between TSH and the cell-membrane cause TSHR to take on the . During this transition, the extracellular LRD rotates 55° along an axis making it perpendicular to the cell membrane. This rotation is initiated by conformational changes within the , specifically at the . Y279 moves 6 Å relative to I486, a residue located in the Transmembrane Region [1]. The active form is favored when . The structure can be seen as straight. The same straight conformation is observed when TSHR is bound with M22. The inactive form is found when of TSHR is found when bound with K1. The overall structure of the molecule is bent when K1 is bound.
Specific Residues and Interactions
There are two in the binding pocket of TSHR that are the main contributors to the binding of the antibodies. The concave structure of the binding pocket allows a with the antibodies. These antibodies make tight interactions with a lot of intermolecular forces at play. interacts with Glu 118 on the antibodies to make a salt bridge interaction. interacts with Asp 111 on the antibodies to make a salt bridge interaction. Specifically, the two residues make an ionic interaction. The interaction is not close enough to make a hydrogen bond. Instead, the interaction between the Lys residues with the Asp or Glu residues is a salt bridge interaction. This is the main bond that holds these two molecules together. When in the inactive form, LYS 209 does not interact with any residue but LYS 58 has interaction with Glu 118 and this interaction pulls the molecule into the bent position. The salt bridge interaction between Lys and Glu is very specific. Lys was mutated with Arg and was expected to make the same salt bride interaction with Glu, however it make a completely different interaction. This new interaction favors a gain of function towards hCG [8].
Biological Relevance
![Figure 4: T3 and T4 role in TSH concentration: Highlighting the problem when under or overactive on the metabolism. When an antibody is bound to TSHR and cannot respond to the negative feedback look the metabolism experiences a shift outside of equilibrium resulting in a wide array of side effects. [2]](/wiki/images/thumb/5/5f/T3t4levels.jpeg/400px-T3t4levels.jpeg)
Figure 4: T3 and T4 role in TSH concentration: Highlighting the problem when under or overactive on the metabolism. When an antibody is bound to TSHR and cannot respond to the negative feedback look the metabolism experiences a shift outside of equilibrium resulting in a wide array of side effects.
[2]The thyroid plays an essential role in the body's metabolism. The body's metabolism affects things like heart rate, digestion, temperature regulation, and many more things. When TSH is bound to TSHR, a signal is sent to produce T3 and T4. T4 is considered an inactive form and needs to be converted into T3 to become active. Those hormones then go impact cells in your body to increase or decrease your metabolism. The T3 and T4 hormones use a feedback system to regulate the release of TSH. When the hormone levels are high they travel through the bloodstream to prevent TSH production. When the hormones are low they are not able to continue the negative feedback loop, thus allowing TSH to be released to bind to TSHR.
Hyperthyroidism
Hyperthyroidism is when the thyroid is overactive which leads to upregulation of the metabolism. This overactive state can be initiated by antibodies like M22. When the M22 antibody is bound it keeps TSHR in the active conformation. When stuck in the active form, the thyroid continues to make T3 and T4, overstimulating the metabolism. Symptoms of hyperthyroidism include fast or irregular heartbeats, tiredness, increased hunger, sleep problems, enlarged thyroid gland, and sensitivity to heat. Grave's Disease is the most common cause of hyperthyroidism. This is an autoimmune disorder that causes your body to attack the thyroid gland[9].
Hypothyroidism
Hypothyroidism is when the thyroid is underactive. The underactive state is initiated when antibodies like K1 are bound. When the K1 antibody is bound it does not allow the TSHR to go into the upright, active, position. This does not allow for the signaling of the T3 and T4 hormones to upregulate the metabolism. When stuck in the inactive form, TSH or M22 cannot bind to the TSHR to make more thyroid hormones which leads to an under-stimulation of the metabolism. The symptoms of this include slow or irregular heartbeats, tiredness, muscle aches, memory problems, jaundice, and sensitivity to cold. Hasimoto's disease is an example of hypothyroidism. This is an autoimmune disorder that causes your body to attack the healthy cells of the thyroid. Specifically causing the death of the cells that produce the thyroid hormones. When the thyroid fails to produce its hormones it activates TSH production through a negative feedback mechanism[9]
![Figure 1: An overview of the Thyroid System. A depiction of signaling cascade from the hypothalamus ending in the release of TSH causing T3 and T4 production and its effects. The mechanism of regulation is also shown by negative feedback from the T3 and T4 hormones. Source: [1]](/wiki/images/thumb/1/1d/TSH_system1.png/300px-TSH_system1.png)
![Figure 4: T3 and T4 role in TSH concentration: Highlighting the problem when under or overactive on the metabolism. When an antibody is bound to TSHR and cannot respond to the negative feedback look the metabolism experiences a shift outside of equilibrium resulting in a wide array of side effects. [2]](/wiki/images/thumb/5/5f/T3t4levels.jpeg/400px-T3t4levels.jpeg)
